Product Hopping: What It Is, Why It Happens, and How It Affects Your Medication Costs
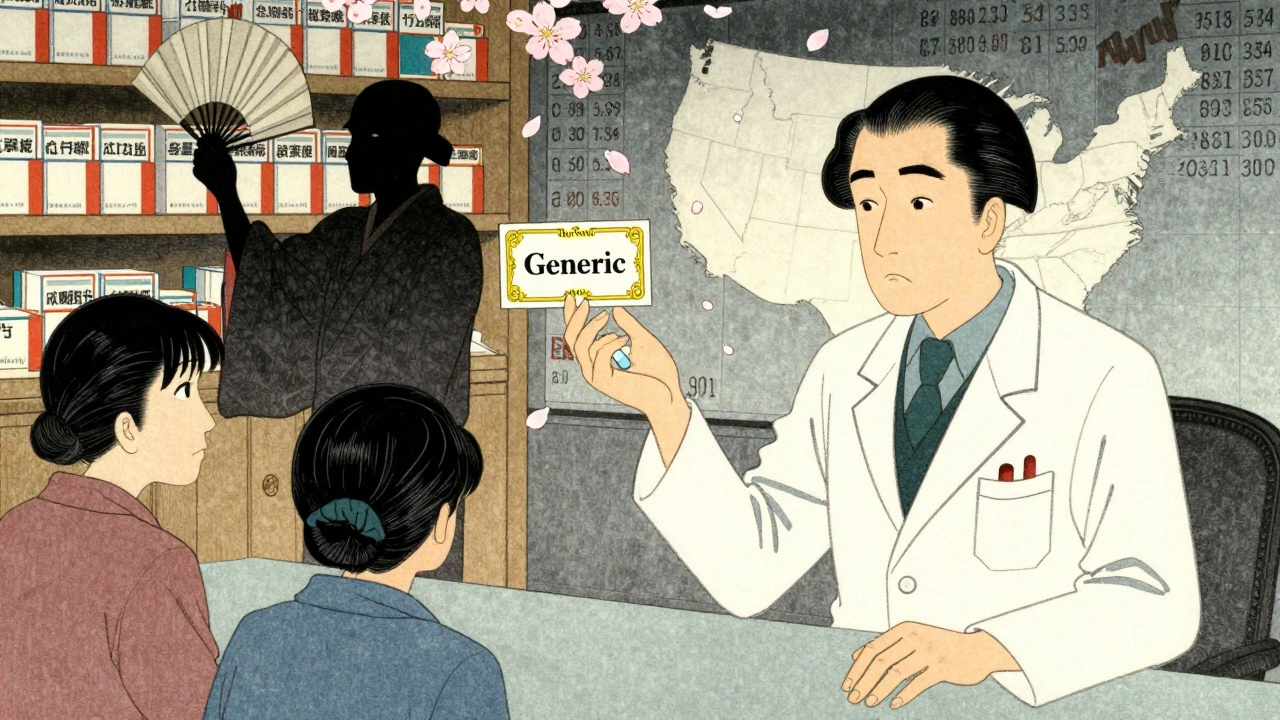
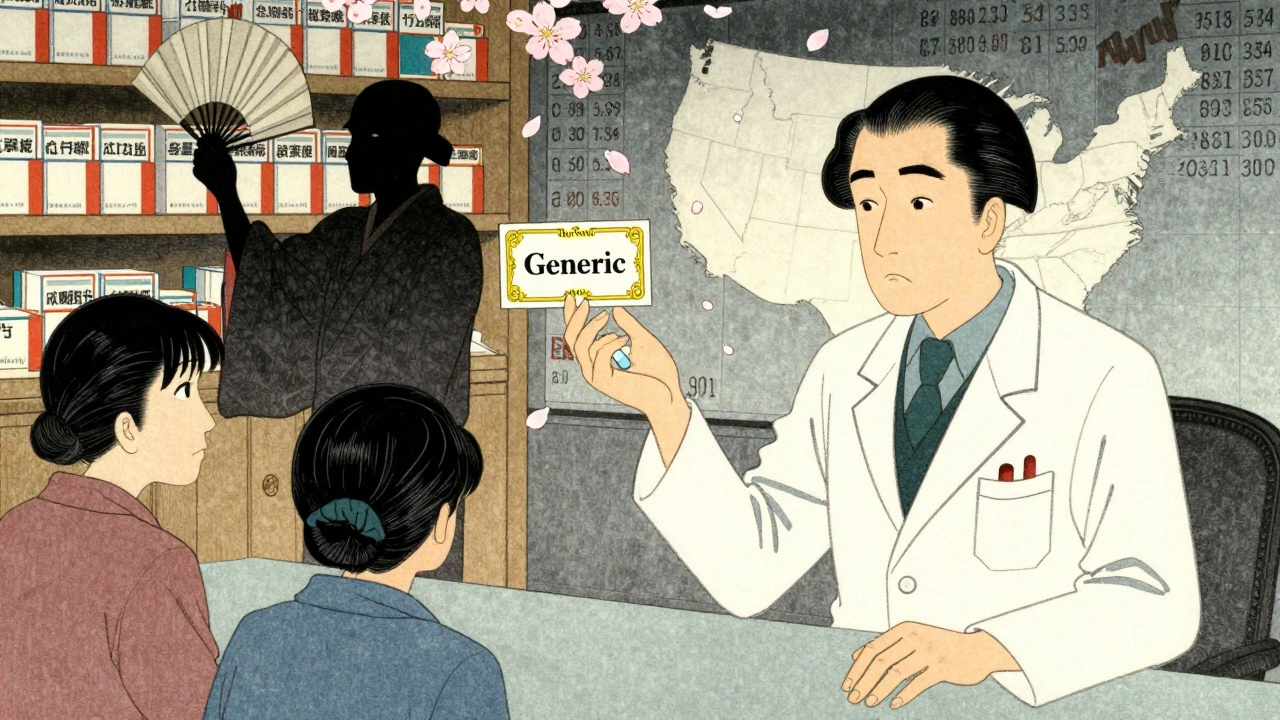
When companies make small changes to an existing drug just to extend its patent life, that’s called product hopping, a strategy where pharmaceutical companies replace an older drug with a slightly modified version to maintain high prices and block generic competition. Also known as drug switching, it’s not about better medicine—it’s about keeping profits high. This isn’t rare. It happens with asthma inhalers, antidepressants, and even cholesterol drugs. The new version might have a different pill shape, a new delivery system, or a tiny dosage tweak. But it’s still the same active ingredient. The goal? Make you switch away from the cheap generic and onto the expensive brand-new version.
Why does this matter to you? Because when a drug goes off-patent, generics should drop the price by 80% or more. But if the company quietly stops making the original and pushes you toward their new version, you’re stuck paying full price. This trick works because doctors often don’t realize the original is gone, and pharmacies can’t substitute the generic if it’s no longer available. generic drugs, lower-cost versions of brand-name medications that contain the same active ingredient and meet the same safety standards become harder to get—not because they’re unsafe, but because the manufacturer removed them from the market. Meanwhile, brand-name drugs, medications sold under a proprietary name by the original developer, often at significantly higher prices than generics keep selling at premium rates. The result? You pay more. Insurance pays more. And the system rewards companies for delaying competition, not improving care.
Some of the posts here show how this plays out in real life. One looks at how statin side effects push patients to switch meds—sometimes because their old version disappeared, not because it stopped working. Another explains how authorized generics work, which is the one legal way to get the exact same drug as the brand, just cheaper. And there’s a deep dive into patent law cases that determine when generics can actually hit the market. These aren’t random topics. They’re all connected to the same problem: when profit drives drug access, not patient need.
You don’t need to be a pharmacist to fight back. Know your meds. Ask if your prescription was switched because it’s better—or because the old one isn’t available anymore. Check if a generic version still exists under a different name. And if your pharmacy says they can’t fill it, ask why. Sometimes, the answer isn’t about safety. It’s about money.
Big Pharma uses legal loopholes like product hopping and REMS abuse to block generic drugs, keeping prices high. Learn how antitrust laws are being used to fight back-and why patients are paying billions more than they should.