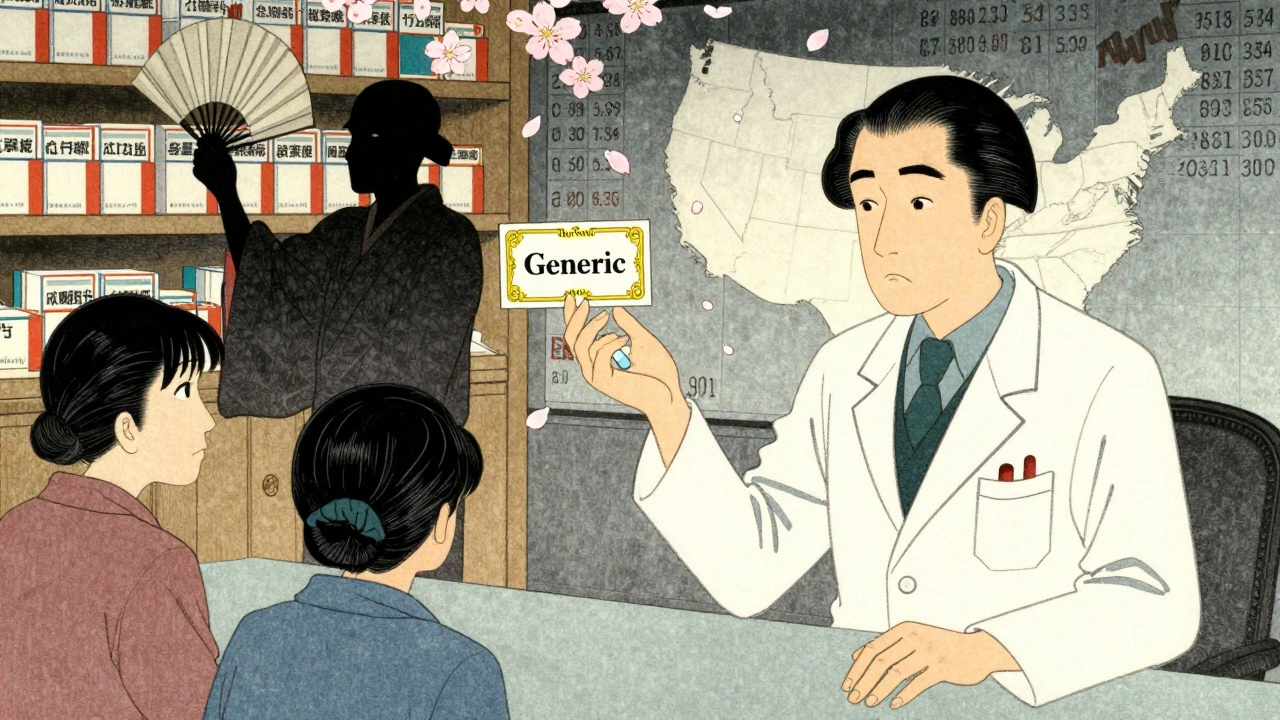
When you pick up a prescription, you expect to get the cheapest effective option available. That’s the whole point of generic drugs: same active ingredient, same effectiveness, but often 80% cheaper. But what if the company that made the brand-name drug actively works to stop you from getting it? That’s not a glitch-it’s a strategy. And it’s happening right now, across the U.S., with the full backing of corporate lawyers and patent filings.
How Generic Substitution Is Supposed to Work
Every state in the U.S. has laws that let pharmacists swap a brand-name drug for a generic version, unless the doctor specifically says "do not substitute." These are called generic substitution laws. They exist to save money-for patients, for insurers, for Medicare and Medicaid. When a patent expires, generic manufacturers can legally copy the drug. Once they enter the market, pharmacists can automatically switch prescriptions. That’s how competition is supposed to work: lower prices, more access. But here’s the problem: brand-name companies don’t wait for generics to show up. They act before that happens. And they don’t just raise prices-they change the product itself to block substitution.Product Hopping: The Hidden Trick
The most common tactic is called product hopping. It’s simple in theory, devastating in practice. A company has a drug with a patent about to expire. Instead of letting generics take over, they introduce a new version-slightly different, often with no real medical benefit-and then pull the original off the market. Take Namenda, a drug for Alzheimer’s. The original version, Namenda IR (immediate release), was due to lose patent protection. Before generics could enter, the manufacturer, Actavis, introduced Namenda XR, an extended-release version. Then, 30 days before generics were allowed to be sold, they stopped making Namenda IR entirely. Why does that matter? Because state substitution laws only apply to the exact same formulation. If the original version isn’t available, pharmacists can’t substitute the generic version of it. Patients are forced to switch to the new version, which is still under patent and still expensive. And once they switch, they rarely go back. Getting a new prescription, adjusting to a new pill form, dealing with insurance-those are all barriers. The FTC called this "eliminating the prescription base for the original product before generics even have a chance to be substituted."How Courts Have Ruled-And Why It’s Inconsistent
Not every product hop works. In 2016, the Second Circuit Court of Appeals ruled in New York v. Actavis that withdrawing Namenda IR was illegal. The court said: "You can’t destroy the market for the original drug just to block generic competition." That was a landmark decision. It recognized that state substitution laws are the only real tool generics have to compete. But not all courts agree. In the In re Nexium case, AstraZeneca switched patients from Prilosec to Nexium, but kept Prilosec on the market. The court dismissed the antitrust claim, saying adding a new product is "procompetitive." The difference? If the old version is still available, courts say it’s fair game. If it’s pulled? That’s anticompetitive. That inconsistency is the problem. One judge sees product hopping as innovation. Another sees it as a legal loophole. And in the meantime, patients pay more.
REMS Abuse: Blocking Generic Access Before It Even Starts
There’s another tactic even less visible: REMS abuse. REMS stands for Risk Evaluation and Mitigation Strategies. These are safety programs the FDA requires for certain high-risk drugs. But some brand-name companies use them as weapons. To get FDA approval, generic makers need samples of the brand-name drug to prove their version is equivalent. But if the brand company refuses to sell those samples-or ties them to restrictive contracts-generics can’t test their product. No test. No approval. No competition. A 2017 study found over 100 generic companies couldn’t get samples for drugs they wanted to copy. One analysis estimated that just 40 drugs with restricted access programs cost the system more than $5 billion a year in lost savings. The FTC called this a "textbook case of monopolization." Why? Because the brand company gains nothing from withholding samples except to delay competition.Real Cases, Real Costs
The numbers don’t lie. In 2023, Drug Patent Watch estimated that just three drugs-Humira, Keytruda, and Revlimid-cost U.S. patients and taxpayers $167 billion in extra spending because generic entry was delayed compared to Europe. Revlimid’s price jumped from $6,000 to $24,000 per month over 20 years. Teva’s switch from Copaxone to a new formulation blocked generics for years. Consumers paid an extra $4.3 to $6.5 billion in that time. In the Suboxone case, Reckitt Benckiser pulled the tablet version and pushed a film version, while spreading false safety claims about the original. The FTC settled with them in 2019 and 2020 after finding the company had coerced patients and doctors into switching. When substitution laws work, generics capture 80-90% of the market within months. When product hopping works? That number drops to 10-20%. That’s not competition. That’s control.

9 Comments
Product hopping isn’t just unethical-it’s a legal farce. The FTC’s 2022 report laid bare the mechanics: companies aren’t innovating, they’re engineering obsolescence. Namenda XR? A placebo with a new pill shape. The Second Circuit got it right-destroying a market to preserve a patent is antitrust 101. And yet, courts like in Nexium still treat this as ‘procompetitive.’ That’s not jurisprudence; that’s corporate capture.
The real tragedy? Patients don’t even know they’re being manipulated. They think they’re getting ‘better’ care when they’re just being herded into more expensive formulations. The FDA’s REMS system was meant for safety, not monopolization. Now, generic manufacturers can’t even get samples to test equivalence. That’s not regulation-that’s sabotage.
And don’t get me started on Humira. $167 billion wasted because a company figured out how to extend a patent by changing the delivery method. That’s not innovation. That’s extortion with a prescription pad.
Okay but what if this is all just a big lie made up by Big Pharma HATERS? Like, what if the ‘new’ versions are actually BETTER? What if the ‘old’ ones had side effects no one talks about? Who says the government even knows what’s safe? Maybe the FDA’s just in the pocket of generic manufacturers who want to cut corners. I’ve seen people get seizures from generics-REAL seizures-and now they’re trying to force them on everyone? This isn’t about price-it’s about control. And who’s controlling WHO?!
Thank you for writing this. I’ve been on a few of these drugs and never realized how much manipulation was going on behind the scenes. My mom switched from the original Copaxone to the new version and ended up paying triple-no one told her she didn’t have to. It’s scary how little patients know. But change is possible. I’ve started sharing this with my support group. We’re writing to our reps. Small steps, but they matter.
It’s not capitalism. It’s feudalism with pill bottles.
The legal inconsistency between New York v. Actavis and In re Nexium is not merely a judicial discrepancy-it reflects a deeper failure in antitrust jurisprudence to adapt to pharmaceutical market dynamics. The concept of ‘product improvement’ as a defense ignores the reality of therapeutic equivalence and the behavioral economics of patient inertia. Courts must recognize that the withdrawal of a non-inferior product, when done strategically to eliminate substitution, constitutes exclusionary conduct under Section 2 of the Sherman Act. The FTC’s recent enforcement actions are a necessary corrective.
I just want to say-this isn’t just about money. It’s about dignity. My brother has MS. He’s been on Copaxone for years. When they switched him to the new version without telling him it was the same drug, he felt like he was being treated like a lab rat. He didn’t want the new one. He didn’t need it. But he had no choice. Please don’t let them keep doing this to people who are already struggling. We’re not just numbers.
Wait so you’re saying the government is letting drug companies lie to people and charge more? That’s wild. I thought we were supposed to be the land of the free? Like, if I try to sell fake sneakers, I go to jail. But if Big Pharma fakes a ‘new’ pill to make you pay more? They get a lobbyist. This is messed up.
Ha! You Americans think you’re so clever with your ‘generic substitution laws’-but you’re just naive. In India, we know better: if you want cheap medicine, you don’t wait for the government or some court to ‘protect’ you-you go to the pharmacy and ask for the active ingredient by name. No brand. No tricks. No patent games. You want generics? Don’t ask for permission-just demand the chemical. Your system is broken because you believe in bureaucracy. We believe in biology. And biology doesn’t care about your patents.
Also, why are you so shocked? The West has been outsourcing its pharmaceutical ethics for decades. You outsource manufacturing, then outsource your outrage. Wake up. This isn’t a conspiracy-it’s capitalism. And capitalism always wins.
By the way, your ‘FTC’? It’s a toothless tiger. In India, we don’t wait for regulators-we take matters into our own hands. We import. We compound. We bypass. You’re still arguing about ‘removal of original product’ while we’re already on the next batch. Your system is a museum. Ours is a revolution.
And yes-I used six exclamation points. Because you need to feel it.
Reading this made me furious-but also hopeful. The fact that the FTC is fighting back, that states are suing, that people are speaking up… it means we’re not powerless. I used to think this was just how the system worked. But now I see it’s not inevitable. It’s chosen. And if enough of us demand change, they’ll have to listen. I’m sharing this with my family. I’m calling my rep. I’m not staying silent anymore.
To everyone who’s been scared to speak up-your voice matters. You’re not alone.