Generic Substitution: What It Means and Why It Matters for Your Medications
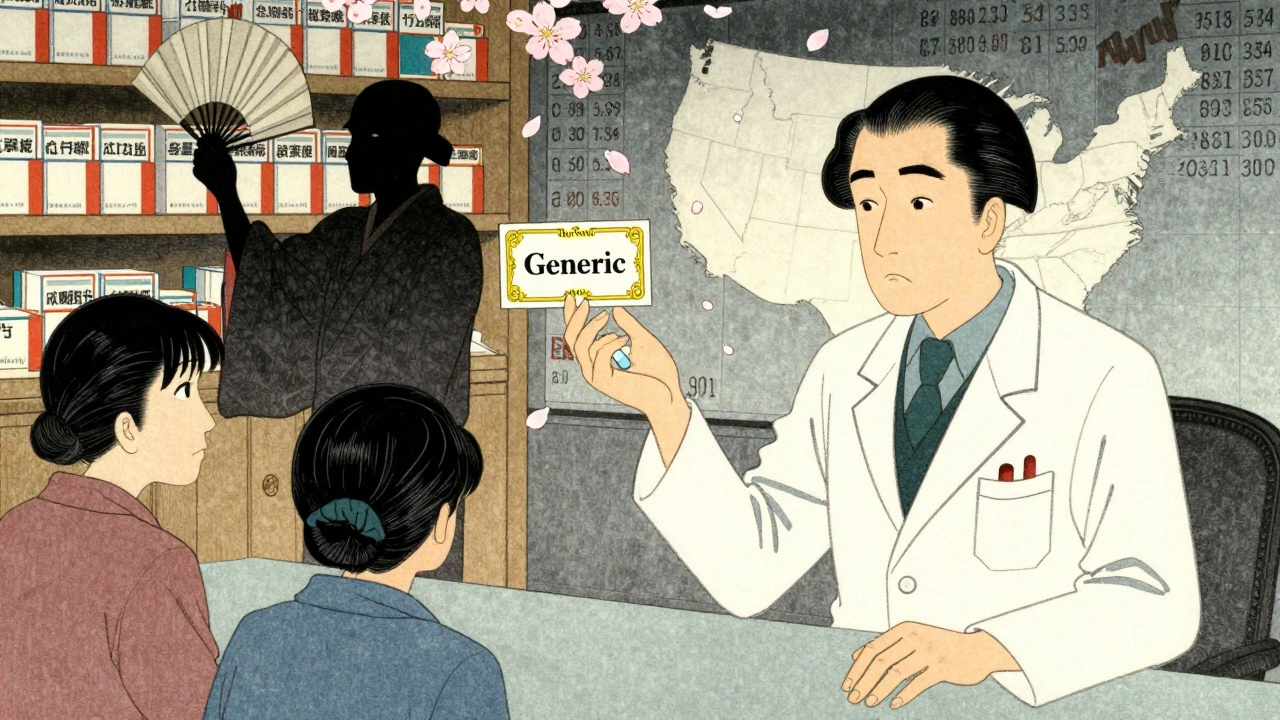
When your pharmacist hands you a different pill than what your doctor prescribed, that’s generic substitution, the practice of swapping a brand-name drug for a chemically identical generic version. Also known as therapeutic substitution, it’s meant to cut costs—but not all substitutions are created equal. For most drugs, it works fine. But for others, even tiny differences in how the body absorbs the medicine can lead to serious problems.
That’s where NTI generics, drugs with a narrow therapeutic index. Also known as narrow therapeutic window drugs, they’re the ones where the difference between a safe dose and a dangerous one is razor-thin. Think warfarin, levothyroxine, or lithium. These aren’t like ibuprofen or metformin. If your body absorbs 10% more or less of the active ingredient, it can mean a blood clot, a thyroid crash, or even toxicity. That’s why the FDA, the U.S. agency that approves drugs and monitors safety. Also known as U.S. Food and Drug Administration, it sets strict bioequivalence rules for these drugs—rules that other countries like the EMA or Health Canada often follow even more tightly.
And then there’s bioequivalence, the scientific standard that proves a generic drug performs the same way in your body as the brand. Also known as pharmacokinetic equivalence, it’s measured by how fast and how much of the drug enters your bloodstream. A generic doesn’t need to be identical in shape or color—but it must deliver the same amount of medicine at the same rate. Most generics pass this test easily. But for NTI drugs, even small variations in fillers, coatings, or manufacturing can break that balance. That’s why some doctors and pharmacists avoid automatic substitution for these meds. They know what happens when you swap levothyroxine brands: patients go from feeling fine to exhausted, shaky, or worse.
Generic substitution isn’t bad. It’s saved billions in healthcare costs. But it’s not a one-size-fits-all system. The posts below show you exactly where it works, where it doesn’t, and how to protect yourself. You’ll see how the FDA and EMA handle substitution differently, why some pharmacies push certain generics over others, and what real patients have experienced when a switch went wrong. Whether you’re on blood thinners, thyroid meds, or just trying to save money on your prescriptions, this collection gives you the facts you need to speak up—or stay safe.
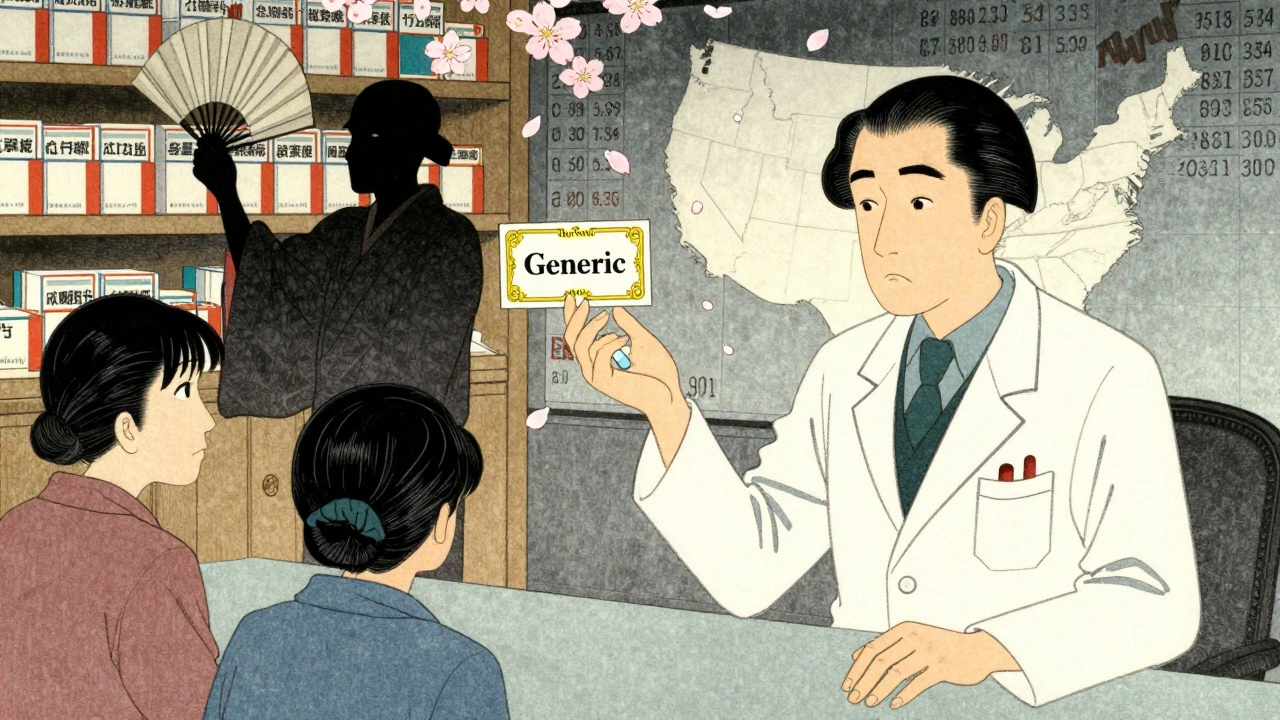
Big Pharma uses legal loopholes like product hopping and REMS abuse to block generic drugs, keeping prices high. Learn how antitrust laws are being used to fight back-and why patients are paying billions more than they should.