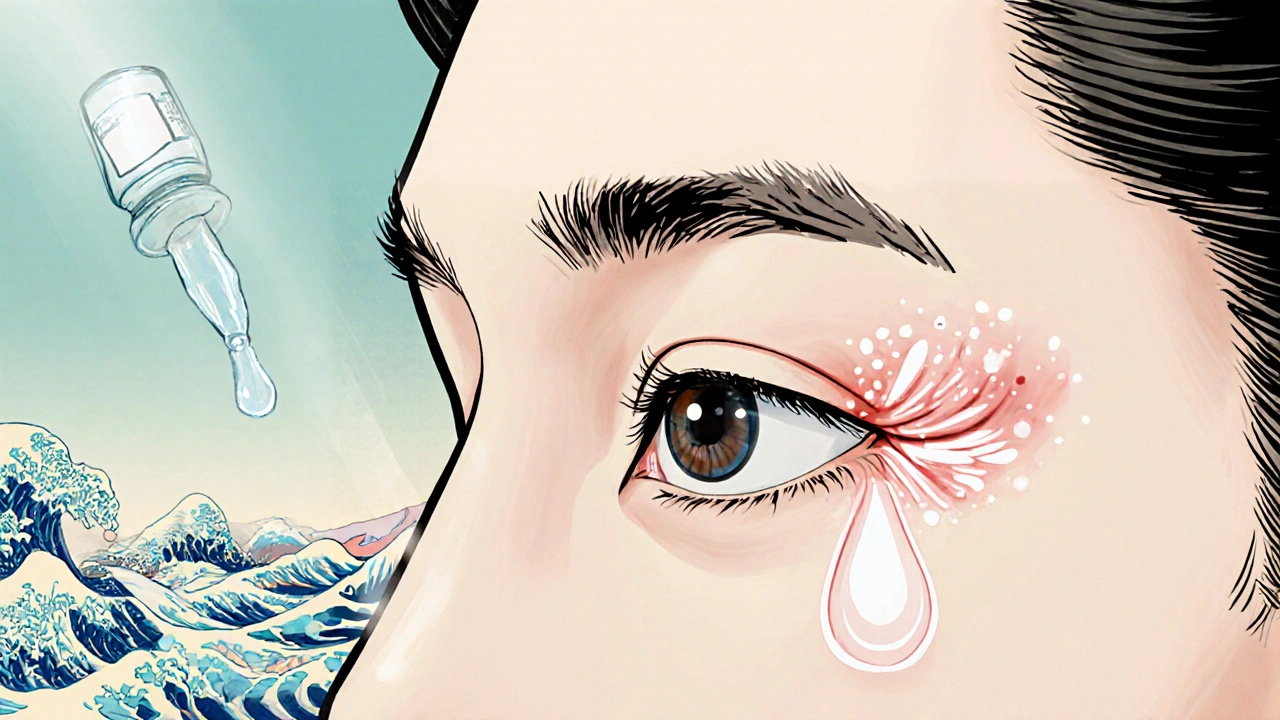
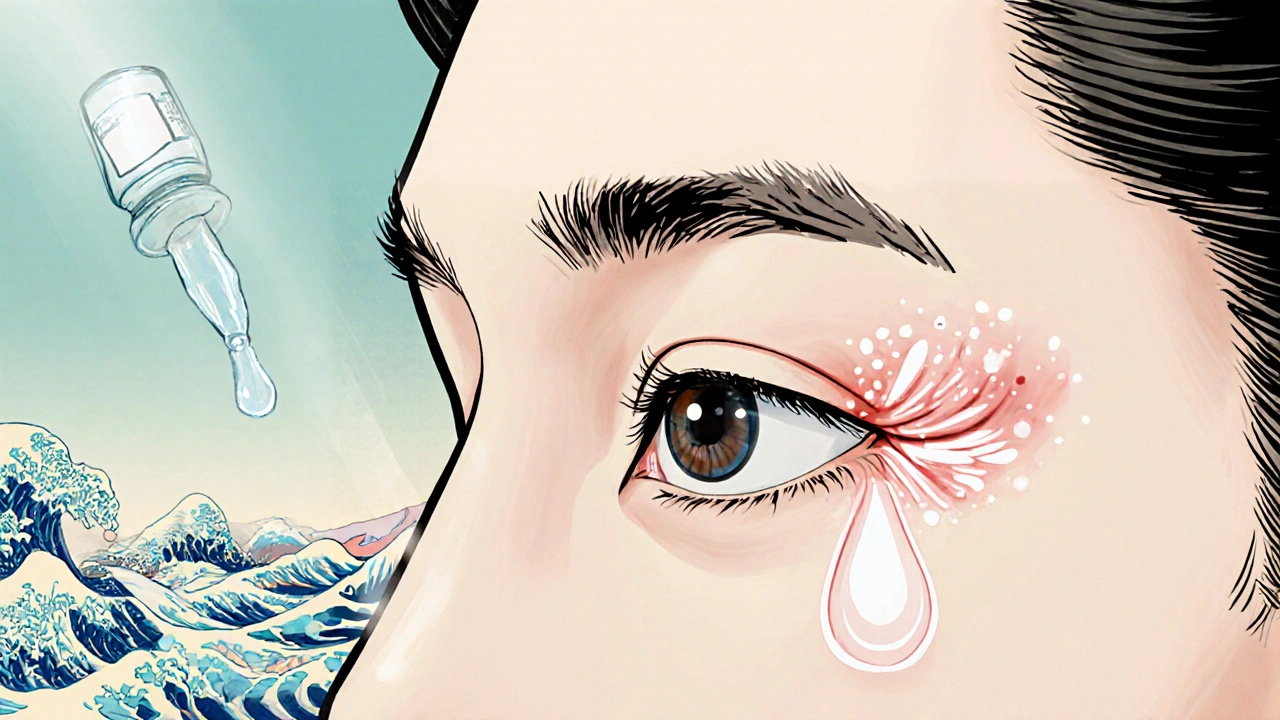
Eye Inflammation Management
When dealing with Eye Inflammation Management, the process of reducing swelling, pain, and redness in the eye caused by various medical conditions. Also known as ocular inflammation control, it aims to preserve vision and comfort. Effective eye inflammation management blends medication, lifestyle tweaks, and monitoring of underlying health issues.
One major driver of eye inflammation is Graves' disease, an autoimmune thyroid disorder that often triggers Graves' ophthalmopathy. This condition inflames the tissues around the eyes, causing bulging, dryness, and vision changes. Managing the eye symptoms without addressing the thyroid imbalance usually falls short, so controlling thyroid hormone levels becomes a core attribute of successful treatment.
Key Factors in Managing Ocular Inflammation
Another related entity is thyroid disorders, which include both hyper‑ and hypothyroidism. These disorders influence blood flow and immune activity, shaping how the eye reacts to inflammation. A typical attribute‑value pair looks like: Entity – Thyroid disorder; Attribute – Hormone imbalance; Value – Elevated T3/T4 or low T4 levels. Adjusting medication, whether antithyroid drugs or hormone replacement, directly reduces ocular swelling.
Stress also plays a surprising role. High cortisol from chronic anxiety can skew immune responses, making the eye’s delicate tissue more prone to flare‑ups. In other words, eye inflammation management often requires stress‑reduction techniques such as mindfulness, regular exercise, or adequate sleep. When stress is tamed, the immune system calms down, and eye irritation lessens.
The immune system itself is a third pillar. Deficiencies in enzymes that support immune health, like zinc‑dependent enzymes, can weaken the body’s ability to control inflammation. Think of it as an entity‑attribute‑value set: Entity – Enzyme deficiency; Attribute – Immune support; Value – Low zinc, low SOD activity. Supplementing with the right nutrients and balancing gut health provides the body with tools to curb eye inflammation from the inside out.
Putting these pieces together forms several semantic triples:
- Eye inflammation management encompasses treatment of Graves' disease‑related eye problems.
- Effective management requires stabilizing thyroid hormone levels.
- Stress influences immune response, which can worsen ocular inflammation.
- Enzyme deficiency weakens immunity, increasing the risk of eye swelling.
- Targeted medication supports the eye’s healing process when underlying causes are addressed.
These connections guide readers toward a holistic view rather than a single‑pill fix.
In practice, doctors often start with a quick assessment: identify the root cause (Graves', thyroid imbalance, stress, or immune weakness), then layer treatments. Corticosteroid eye drops or oral steroids can rapidly calm acute swelling, but they’re paired with long‑term strategies like thyroid medication adjustment, stress management, and nutritional support. Monitoring tools such as intra‑ocular pressure checks and visual acuity tests help track progress and catch complications early.
Below you’ll find a curated set of articles that dive deeper into each of these aspects—whether you’re looking for alternative therapies for Graves' disease, ways stress triggers eye issues, or how enzyme health ties into immunity. The collection offers practical steps, safety tips, and the latest research to empower you in mastering eye inflammation management.
A practical, step‑by‑step guide to controlling eye inflammation after surgery at home, covering drops, cold therapy, monitoring signs, and when to seek help.