Post-Surgical Eye Inflammation Symptom Checker
This interactive tool helps you determine if your symptoms after eye surgery indicate normal inflammation or if you should contact your surgeon immediately. Based on the red-flag symptoms described in the article, please answer the following questions.
Note: This tool is for educational purposes only and should not replace professional medical advice.
Answer the questions above to see if you need to contact your surgeon.
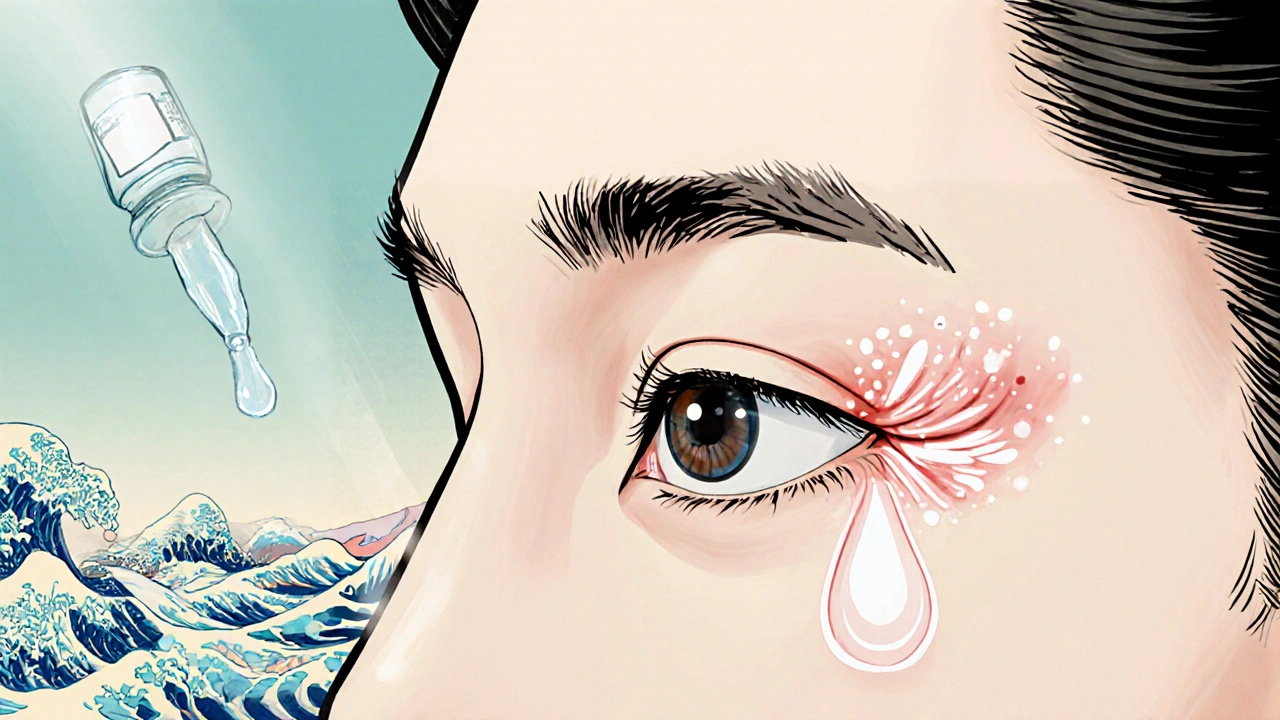
Postoperative ocular inflammation is a common reaction that occurs after eye procedures such as cataract removal, LASIK, or retinal surgery. It typically shows up as redness, swelling, mild pain, and blurry vision within the first 24‑48 hours. While doctors prescribe drops to keep the reaction in check, most of the recovery happens at home. This guide walks you through the day‑to‑day steps that keep the inflammation under control, so you can get back to reading, driving, and scrolling without unnecessary worry.
Key Takeaways
- Start a structured medication schedule the moment you get home - missing a dose can let inflammation spike.
- Cold compresses for 10‑15 minutes, three times a day, dramatically cut swelling.
- Regularly check the eye with a fluorescein stain (or a bright‑light inspection) to spot persistent irritation.
- Watch intraocular pressure (IOP) signs: persistent headache, halos around lights, or worsening vision need urgent review.
- Know the red‑flag symptoms that require a call to your surgeon or an emergency eye clinic.
What Exactly Is Post‑Surgical Eye Inflammation?
After any intra‑ocular operation, the body treats the incision like a tiny wound. White blood cells flood the area, releasing cytokines that cause the classic redness and swelling. In most cases the reaction peaks around day 2‑3 and then tapers off. The degree of inflammation depends on the type of surgery, the surgeon’s technique, and how well you follow post‑op instructions.
Two drug families dominate the treatment plan:
- Corticosteroid eye drops - powerful anti‑inflammatory agents that slow the immune response.
- NSAID eye drops - non‑steroidal anti‑inflammatory drugs that reduce swelling without raising intraocular pressure.
Both are usually prescribed together for the first week, then tapered according to your surgeon’s schedule.
Typical Symptoms and When They Appear
Most patients experience a mix of these signs:
- Redness around the cornea and conjunctiva.
- Swelling of the eyelids - they may look puffy or feel tight.
- Mild to moderate eye pain, often described as a gritty sensation.
- Blurred or fluctuating vision, especially in low light.
- Increased tearing or a watery discharge.
If any of these symptoms worsen after the third postoperative day, it may signal infection or a pressure problem rather than just inflammation.
Why Home Management Is Crucial
Doctors can’t be at your side 24/7, and the eye heals fastest when you stick to a disciplined routine. Consistency with drops, cold therapy, and hygiene dramatically lowers the odds of complications like uveitis, cystoid macular edema, or pressure spikes.
Moreover, the psychological comfort of knowing exactly what to do each day reduces anxiety and helps you sleep better - a hidden factor that speeds tissue repair.

Day‑One Checklist: The First 24 Hours
When you get home, you’ll likely have a small vial of postoperative eye inflammation medication, a shield, and a pack of sterile gauze. Follow this checklist before you even think about TV:
- Set up a medication timer. Use your phone’s alarm or a pill‑reminder app. Typical schedule: one drop of steroid, one drop of NSAID, and one drop of antibiotic every 2-4 hours while awake.
- Apply a cold compress. Wrap a clean cloth around a bag of frozen peas, then place it gently over the closed eye for 10‑15 minutes. Do this three times today - morning, afternoon, and evening.
- Wear the protective eye shield. Most surgeons give a molded shield that you keep on while sleeping. It prevents accidental rubbing and shields the eye from drafts.
- Keep the eye clean. Gently wipe away any discharge with a sterile cotton swab, moving from the inner corner outward. Never share towels.
Document the exact time you give each drop. A simple notebook or a notes app works fine.
Medication Overview & Comparison
Below is a quick look at the most common drops used after eye surgery. Your surgeon will choose the exact brand, but the core attributes stay the same.
| Feature | Corticosteroid (e.g., prednisolone) | NSAID (e.g., ketorolac) |
|---|---|---|
| Primary action | Suppresses immune cascade | Inhibits prostaglandin synthesis |
| Typical dosage | 1‑2 drops every 2‑4 h | 1‑2 drops every 4‑6 h |
| Effect on IOP | May raise pressure in steroid‑responders | Neutral to modestly lowers pressure |
| Common side‑effects | Increased eye pressure, delayed wound healing | Transient burning sensation |
| Typical taper period | 1‑2 weeks, then gradual reduction | Usually stopped after 1 week |
Tip: If you’ve ever been told you’re a “steroid responder” (your eye pressure spikes with steroids), your doctor may favor NSAID drops or add a pressure‑lowering medication.
Non‑Medication Strategies That Really Work
Medication does most of the heavy lifting, but these simple habits shave days off recovery:
- Cold compresses. The vasoconstriction caused by cold reduces fluid leakage into the tissues, cutting swelling by up to 40 % in the first 48 hours.
- Humidifier. Dry indoor air can exacerbate irritation. Keeping humidity at ~45 % eases discomfort, especially if you use a mask after surgery.
- Elevate your head while sleeping. A pillow‑wedge prevents blood from pooling around the eye, which can worsen puffiness.
- Limit screen time. Blue light can increase tear film instability. Use a screen‑filter and take 20‑second breaks every 20 minutes.
- Stay hydrated. Adequate fluid intake supports overall tissue healing and keeps the ocular surface moist.

Monitoring Your Recovery: Simple Checks You Can Do Daily
Use these quick self‑assessments to catch problems early:
- Visual clarity. Read a line of text on your phone. If letters appear fuzzy for more than 15 minutes after a drop, note it.
- Redness grading. Compare the operated eye to the fellow eye. Mild pink is normal; deep crimson or spreading redness needs a call.
- Pressure sensation. A feeling of “ballooning” behind the eye, or halos around lights, may hint at high IOP.
- Discharge color. Clear or slightly watery is fine. Yellow, green, or foul‑smelling fluid signals infection.
Document these observations in the same notebook you use for drops. A pattern over two days is more telling than a single anomaly.
When to Call Your Surgeon (or Emergency Eye Service)
Most post‑op irritation resolves on its own, but these red‑flags merit immediate attention:
- Severe pain that doesn’t improve with prescribed drops.
- Sudden vision loss or a large dark spot in your visual field.
- Rapidly increasing redness that spreads to the bridge of the nose.
- Persistent fever (>38 °C) alongside eye symptoms.
- Visible swelling of the eyeball itself (proptosis) or feeling of pressure inside the eye.
When you call, have the following ready: surgery date, drop schedule, and a brief symptom timeline. Many clinics now offer telemedicine follow‑up - a quick video can let the surgeon see the eye without you traveling.
Putting It All Together: A 7‑Day Home Recovery Planner
| Day | Medication | Non‑med Actions | Check‑points |
|---|---|---|---|
| 1 | Corticosteroid & NSAID every 2‑4 h; Antibiotic every 4 h | Cold compress 3×, eye shield at night, humidifier on | Redness mild, pain 2/10, vision clear enough for reading |
| 2 | Continue same schedule; begin tapering steroid to every 4 h if instructed | Elevate head while sleeping, hydrate, limit screen to 2 h | Swelling reduced, no new discharge |
| 3 | Drop frequency as per doctor (often 4 h) | Cold compress 2×, gentle eyelid massage with clean cotton | Check IOP signs - no halos, no headache |
| 4‑5 | Begin steroid taper (every 6‑8 h), continue NSAID | Resume light reading, keep humidifier | Vision stabilizes, redness fades |
| 6‑7 | Stop antibiotic, only NSAID once daily if needed | Remove shield, normal sleep positions | Final check - no pain, no new redness, comfortable vision |
After week one, most patients feel comfortable returning to normal activities, but keep the eye shield handy for the next 2‑3 days if you’re in dusty or windy environments.
Bottom Line
Managing postoperative eye inflammation at home boils down to three pillars: disciplined drop schedule, targeted cold therapy, and vigilant self‑monitoring. Pair those with simple lifestyle tweaks - hydration, humidity, and proper sleep posture - and you dramatically lower the odds of complications. Remember, the eye is delicate, but it also heals quickly when you give it the right environment.
How long does postoperative eye inflammation usually last?
Most inflammation peaks around day 2‑3 and subsides significantly by day 7. Mild residual redness can linger for up to two weeks, but it should keep improving.
Can I use over‑the‑counter eye drops for the swelling?
No. OTC artificial tears or decongestant drops don’t target the immune response that causes postoperative swelling. Stick to the prescribed corticosteroid or NSAID drops.
Is it safe to wear contact lenses during recovery?
Generally, no. Most surgeons ask patients to avoid contacts for at least 2‑4 weeks after intra‑ocular surgery to prevent irritation and infection.
What does a rapid increase in eye pressure feel like?
You may notice a throbbing headache, blurry vision with halos around lights, or a sensation of the eye being “full.” If any of these appear, call your surgeon immediately.
How can I tell if my eye infection is getting worse?
Watch for yellow or green discharge, increasing pain, swelling spreading beyond the eyelid, or fever. Those signs mean you need urgent medical review.

14 Comments
Hey there, congrats on getting through surgery! 🎉 The recovery plan might look intense, but you’ve got this. Stick to the drop schedule like a metronome and keep those cold packs coming-trust me, they work wonders. Remember to log everything; a quick note can save you a call later. Stay positive and give yourself credit for each small win!
The article drags on with redundant points and could use a tighter focus. A concise bullet list would serve better than the drawn‑out prose.
I hear you on the need for brevity, but the detail actually helps newcomers who aren’t familiar with ocular physiology. It’s better to have a comprehensive reference than to leave readers guessing about crucial signs like pressure spikes.
Well the layman needs the granularity lest they wander into ignorance its a safe harbor for the uninformed
Honestly this guide hits all the right notes – the step‑by‑step checklist feels like a lifeline after surgery. The drama of day‑by‑day recovery is captured perfectly, and the warnings are spot‑on.
its good but i wish it was shorter
Post‑operative ocular inflammation represents a quintessential example of iatrogenic tissue response mediated by a cascade of cytokine release and leukocyte infiltration. The resultant vasodilation and increased vascular permeability manifest clinically as hyperemia, edema, and nociceptive discomfort. Empirical evidence underscores that the temporal profile of this inflammatory surge typically culminates within the second to third postoperative day, after which a gradual attenuation ensues. Nevertheless, the heterogeneity of patient-specific factors-such as age, comorbid systemic inflammation, and surgical technique-imparts variability to both the magnitude and duration of the response. The concomitant administration of corticosteroid and NSAID eye drops leverages synergistic mechanisms: the former suppresses transcriptional activation of inflammatory genes, while the latter attenuates prostaglandin synthesis at the cyclooxygenase level. Tapering protocols must be calibrated to mitigate the risk of rebound inflammation and to preempt steroid‑induced intra‑ocular pressure elevation. Clinical monitoring protocols frequently incorporate fluorescein staining to delineate epithelial integrity, supplemented by tonometry to detect subclinical pressure spikes. The integration of adjunctive non‑pharmacologic measures-namely cryotherapy via cold compresses, ambient humidity control, and head‑elevation-serves to augment venous outflow and reduce interstitial fluid accumulation. Patient adherence to a rigorously timed drop schedule is paramount; pharmacokinetic modeling suggests that suboptimal dosing intervals may precipitate episodic inflammatory flares. Documentation of drop administration times, symptomatology, and visual acuity fluctuations facilitates objective trend analysis and informs therapeutic adjustments. Moreover, the psychological dimension of recovery, encompassing patient anxiety and perceived control, exerts a measurable influence on healing trajectories, as elucidated by psychoneuroimmunological studies. In the context of potential complications such as cystoid macular edema or infectious endophthalmitis, early detection hinges upon vigilant self‑assessment and prompt communication with the operating surgeon. It is advisable to maintain a low threshold for reporting new-onset pain, visual distortion, or atypical discharge. While the majority of postoperative inflammatory processes resolve spontaneously within a fortnight, persistent residual redness may linger and should be interpreted within the broader clinical picture. Ultimately, an evidence‑based, multimodal approach that synergizes pharmacotherapy, physical measures, and patient education optimizes outcomes and minimizes the likelihood of adverse sequelae.
While the exposition is exhaustive, a succinct summary table would distill the key takeaways for clinicians pressed for time.
Embarking on the post‑surgical recovery journey can feel akin to navigating a labyrinth of instructions, yet each step you take is a deliberate stride toward restored visual acuity. By anchoring your daily routine to the structured medication timetable, you create a predictable pharmacologic rhythm that harmonizes with the eye’s intrinsic healing cadence. The disciplined application of cold compresses three times daily not only curtails edema but also offers a momentary respite, allowing you to pause and assess your comfort level. Maintaining a humid environment mitigates tear film disruption, thereby reducing the gritty sensation that many patients report during the early postoperative phase. Elevating the head of your bed promotes venous drainage, which can subtly diminish periorbital puffiness and improve overall sleep quality. It is equally important to monitor visual clarity by reading a line of text after each drop; any lingering blur may signal the need for dosage adjustment under professional guidance. Should you notice any of the red‑flag symptoms-such as escalating pain, sudden vision loss, or a halo effect around lights-act swiftly by contacting your surgeon, as early intervention can forestall more serious complications. In essence, the convergence of pharmacologic diligence, lifestyle modifications, and proactive self‑monitoring constitutes the cornerstone of an uncomplicated recovery, empowering you to resume daily activities with confidence.
Sounds solid but honestly most people just skip the humidifier and still do fine.
Listen up-stop second‑guessing the drop schedule and just crush it. Your eyes need that exact timing, no excuses. If you miss a dose, double‑check the next one and stay relentless. Consistency is the only weapon you have against inflammation, so grip it and don’t let anything slip.
Whoa, chill, you’re coming on too hard for a simple post‑op routine.
Great rundown! 👍 If you’re curious about how to track intra‑ocular pressure at home, a handheld tonometer can be a game‑changer, though you’ll need a prescription. Also, pairing your cold compresses with a brief 5‑minute eye massage can enhance lymphatic drainage. Just remember to keep the massage gentle to avoid disturbing the surgical site.
While the suggestion of a handheld tonometer is technically feasible, insurance coverage and calibration standards often limit its practicality for postoperative patients; therefore, routine in‑office IOP checks remain the gold standard.