
Most people think if something is natural, it’s safe. That’s why so many take turmeric for joint pain, garlic pills for heart health, or St. John’s wort for low mood-without saying a word to their doctor. But here’s the hard truth: supplements and herbal remedies aren’t harmless snacks. They’re powerful substances that can interfere with your prescriptions, worsen conditions, or even cause dangerous bleeding, heart issues, or organ damage. And if your doctor doesn’t know you’re taking them, they can’t protect you.
Most People Don’t Tell Their Doctors-And It’s Risky
A 2018 study found that only 13% of people told their primary care doctor about their herbal supplements. Even among patients with multiple chronic conditions-people on five or more medications-the disclosure rate barely reached 51%. That means nearly nine out of ten people are taking something that could clash with their heart meds, blood thinners, or antidepressants, and their doctor has no idea. Why? Many assume their doctor won’t care. Others think, “It’s just a vitamin.” Some fear being judged. One patient on Reddit shared how they only mentioned taking garlic pills after nearly bleeding out during minor surgery. Their doctor had never asked. Another person on HealthUnlocked waited two years to tell their cardiologist about turmeric-until he specifically asked. That’s when he warned them: turmeric can thin your blood just like warfarin.What You’re Taking Might Be More Powerful Than You Think
Herbal remedies aren’t tea. They’re concentrated plant extracts with active chemicals that behave like drugs. St. John’s wort, for example, is used for mild depression-but it can cut the effectiveness of birth control pills, HIV meds, and even chemotherapy drugs. It works by speeding up how your liver breaks down other medications. That means your pills stop working. You could get pregnant. Your cancer treatment could fail. Ginkgo biloba, often taken for memory, can increase bleeding risk. If you’re on aspirin or warfarin, combining it with ginkgo can lead to bruising, nosebleeds, or worse-brain bleeds. Even common supplements like vitamin E or fish oil can thin your blood. And if you’re scheduled for surgery, that’s a serious problem. And it’s not just herbs. High-dose zinc can interfere with antibiotics. Calcium supplements can block thyroid meds. Iron pills make your blood pressure drugs less effective. These aren’t rare cases. They’re documented in medical journals. The FDA doesn’t test supplements before they hit shelves. Manufacturers don’t have to prove they’re safe with other drugs. You’re the only one checking.Doctors Don’t Always Ask-But They Should
Most doctors don’t bring up supplements because they’re not trained to. A 2021 survey found only 27% of physicians felt confident discussing them. They’re pressed for time-average appointments last 15 to 20 minutes. They’re focused on blood pressure, cholesterol, diabetes. Supplements? They assume you’d mention it if it mattered. But here’s the problem: patients rarely volunteer this info. They don’t think it’s “medicine.” They don’t realize it’s part of their health picture. That’s why some clinics now use a simple five-question screening tool during intake. It asks: “Are you taking any vitamins, minerals, herbs, or supplements? What are they? Why are you taking them? Have you noticed any side effects? Have you told anyone else about them?” When used, disclosure rates jumped from 33% to 78%. Your doctor isn’t trying to shut you down. They’re trying to keep you alive. If you’re on blood pressure meds and start taking hawthorn berry (a popular heart supplement), your BP could drop too low. You could faint. You could fall. Your doctor needs to know to adjust your dose-or advise you to stop.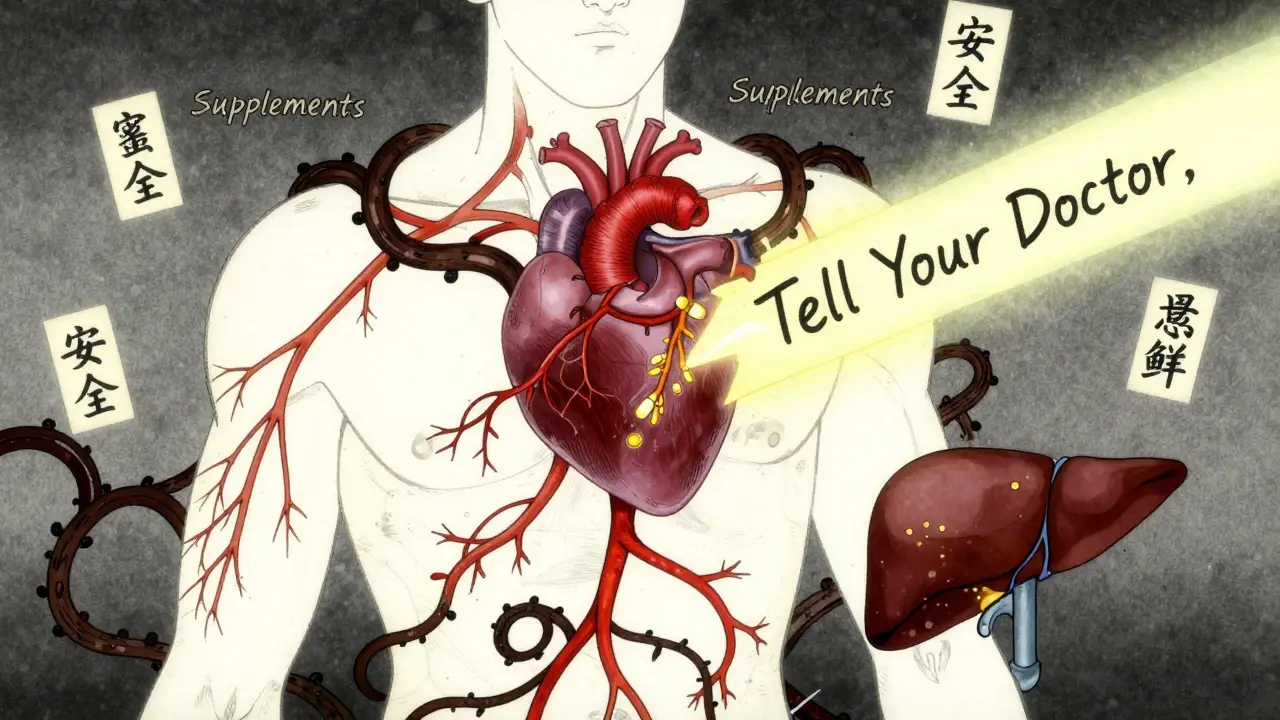
What to Bring to Your Appointment
Don’t rely on memory. Don’t say “I take the red bottle.” Bring the actual bottles. Or take a photo of the labels. Write down the names, doses, and how often you take them. Include everything-even the ones you think are “just for immunity” or “not really medicine.” If you’re unsure what’s in a product, check the label. By law, it must list every ingredient and include this line: “Not evaluated by the FDA. Not intended to diagnose, treat, cure, or prevent any disease.” That’s your warning. It’s not a badge of safety. It’s a legal shield for the company. Some supplements have multiple names. For example, milk thistle is also called Silybum marianum. Kava is sometimes sold as Piper methysticum. If your doctor doesn’t recognize the brand name, the scientific name helps. A picture of the bottle is even better.What Happens When You Do Disclose?
You might worry your doctor will tell you to quit. But that’s not what usually happens. A 2022 survey of 1,200 supplement users found that 78% of those who disclosed got helpful advice. Sixty-three percent said it improved their trust in their provider. Your doctor might say: “Stop the turmeric before your surgery.” Or: “Take the iron two hours apart from your thyroid pill.” Or: “St. John’s wort won’t help your anxiety if you’re on SSRIs-it could make you sick.” They might suggest safer alternatives. Or they might say, “Keep taking it, just monitor for X side effect.” This isn’t about control. It’s about collaboration. You’re not being judged. You’re being protected.Why This Matters More Than Ever
The supplement industry is booming. In 2022, Americans spent over $55 billion on these products. There are more than 85,000 different supplements on the market. Many contain ingredients not listed on the label. Some have hidden drugs-like weight-loss pills laced with stimulants, or erectile dysfunction supplements with hidden sildenafil (the active ingredient in Viagra). The FDA only steps in after harm is done. They don’t approve supplements before sale. They can’t. That’s the law. So the burden falls on you. You’re the first and last line of defense. And it’s not just about you. If you’re on Medicare, you’re part of a group where 67% of users take supplements. That’s millions of people mixing natural products with powerful drugs. Without disclosure, the risk multiplies.
How to Start the Conversation
You don’t need to wait for your doctor to ask. Say it yourself. At your next visit, say:- “I’ve been taking [name] for [reason]. I didn’t think I needed to tell you, but now I’m wondering if it’s safe with my other meds.”
- “I’m taking a few supplements. Can we check if they interact with anything I’m on?”
- “I brought the bottles. Can you help me understand if any of these could be risky?”
What If You’ve Already Had a Reaction?
If you’ve felt dizzy after taking a supplement, had unusual bruising, or noticed your meds stopped working-don’t wait. Tell your provider immediately. Even if it happened months ago. Even if you thought it was “just a coincidence.” Serious reactions from supplements are underreported. The FDA estimates only 1% of adverse events are ever reported. That means most cases go unnoticed. But if you speak up, you help others too. Your story could prevent someone else’s hospital stay.Final Thought: You’re the Expert on Your Body
Your doctor knows medicine. But you know what you feel. You know when your sleep changed after taking ashwagandha. You know when your headaches stopped after starting magnesium. You know when your stomach felt off after the new herbal blend. That knowledge is valuable. But it’s only useful if it’s shared. The gap between what you take and what your doctor knows is where harm happens. Closing that gap isn’t about obedience. It’s about safety. It’s about respect-for your body, your treatment, and your future.Don’t wait for them to ask. Don’t assume it’s not important. Don’t believe “natural” means “safe.” Bring the bottles. Say the names. Ask the questions. Your life might depend on it.
