
Vancomycin Infusion Calculator
Calculate Safe Infusion Time
Enter the vancomycin dose to determine the minimum safe infusion time to prevent infusion reactions.
Infusion Results
Enter a vancomycin dose to see recommended infusion time.
When vancomycin is given too fast, your skin can turn red, feel itchy, and even drop your blood pressure. It’s not an allergy. It’s not rare. And it’s completely preventable. For decades, this reaction was called red man syndrome-a term that’s now outdated, offensive, and medically inaccurate. Today, it’s properly called vancomycin infusion reaction or vancomycin flushing syndrome. If you or someone you know is getting vancomycin, understanding this reaction could mean the difference between a smooth treatment and a scary, avoidable emergency.
What Exactly Is a Vancomycin Infusion Reaction?
Vancomycin infusion reaction (VIR) happens when the antibiotic is infused too quickly. It’s not an allergic reaction. It’s an anaphylactoid reaction-meaning your body releases histamine without being sensitized first. That’s why you can get it on your very first dose. Histamine floods your system, causing blood vessels to widen and skin to flush. This isn’t a sign your body is rejecting the drug. It’s a physical response to speed, not substance.
The classic signs show up 15 to 45 minutes after starting the IV. You’ll notice redness on your face, neck, chest, and upper back. It can feel like a bad sunburn. Itching is common. Some people get a feeling of warmth spreading across their skin. In worse cases, your heart races, your blood pressure drops, or you feel chest tightness or muscle cramps. Breathing problems? Rare. That’s usually a sign of true anaphylaxis, not VIR.
Studies show this reaction isn’t random. In one 1988 study, 9 out of 11 healthy adults got a reaction after getting 1,000 mg of vancomycin over just one hour. None had a reaction when the same dose was given slowly. The faster the infusion, the higher the risk. Infusing vancomycin at more than 10 mg per minute triggers this reaction in most people. Slow it down to 10 mg per minute or slower-meaning a 1,000 mg dose takes at least 100 minutes-and you prevent it in nearly every case.
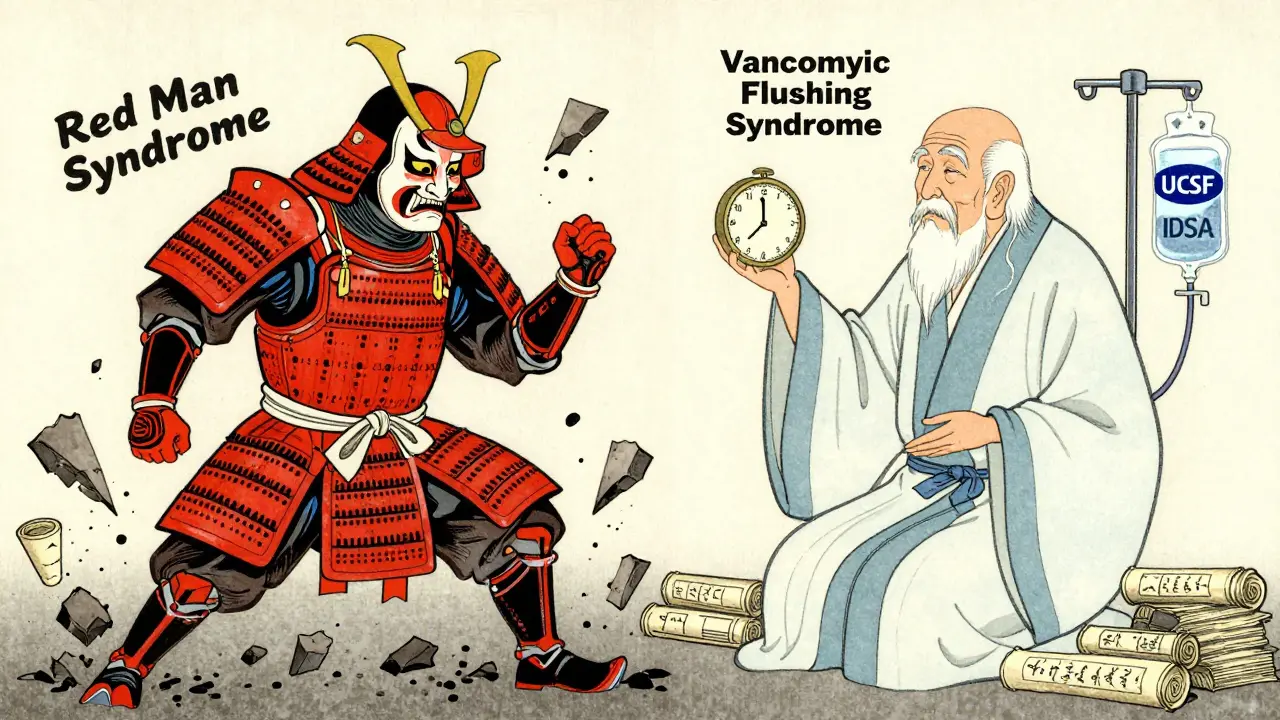
Why the Term ‘Red Man Syndrome’ Is Outdated-and Harmful
The old name, ‘red man syndrome,’ was never medically accurate. It was also racially insensitive. The term implied a visual stereotype, suggesting the reaction was only seen in white people. That’s not true. The reaction happens regardless of skin tone. It’s just more visible on lighter skin.
In 2021, a study in Hospital Pediatrics reviewed over 21,000 patient records. They found that 61.6% of vancomycin allergy entries still used the term ‘red man syndrome.’ After hospitals replaced it with ‘vancomycin flushing syndrome’ in their electronic systems, the use of the old term dropped by 17% in just three months. Institutions like UCSF, Harvard, and the Infectious Diseases Society of America now require the correct terminology in all documentation. The American Academy of Allergy, Asthma & Immunology supports this change as part of a broader effort to remove racist language from medical practice.
Using outdated terms doesn’t just offend-it misleads. If a patient’s chart says ‘allergy to vancomycin’ because of a past flushing reaction, they might be denied a life-saving drug. That’s dangerous. Correct terminology saves lives.
How to Tell It Apart from a True Allergy
Many patients are labeled ‘allergic to vancomycin’ when they’ve never had a true allergic reaction. A 2022 UCSF guideline studied 198 patients with reported vancomycin allergies. Only 3% had true IgE-mediated anaphylaxis. Another 4% had severe skin reactions like DRESS, SJS, or TEN-these are real allergies. But the vast majority-over 90%-had vancomycin infusion reaction.
Here’s how to tell the difference:
- VIR: Flushing on face, neck, chest. Itching. No swelling. No wheezing. No drop in oxygen. Happens during or right after infusion. Can happen on first dose.
- True Anaphylaxis: Swelling of lips or throat. Wheezing. Difficulty breathing. Low blood pressure. Can be fatal. Requires prior exposure. Involves IgE antibodies.
One big clue? If you’ve had a reaction before and got vancomycin again-slowed down-and didn’t react, it was likely VIR, not allergy. True allergies don’t go away with slower infusions.
How to Prevent It
Prevention is simple. And it’s not about drugs. It’s about time.
The gold standard: Infuse vancomycin at 10 mg per minute or slower. That means:
- 500 mg → at least 50 minutes
- 1,000 mg → at least 100 minutes
Some hospitals give 1,000 mg over 90 minutes. Others stretch it to 120 minutes for extra safety. Either way, don’t rush it. Don’t use a pump set to deliver it in 30 minutes. That’s asking for trouble.
Also, avoid giving vancomycin at the same time as other drugs that trigger histamine release. That includes:
- Opioids (like morphine or fentanyl)
- Neuromuscular blockers (like succinylcholine)
- Radiocontrast dye
These drugs can make the reaction worse. Give them hours apart, if possible.
What to Do If a Reaction Happens
If flushing, itching, or redness starts during the infusion:
- Stop the IV immediately.
- Notify the medical team.
- Check vital signs-blood pressure, heart rate, oxygen levels.
- Most reactions resolve within 30 minutes after stopping the drip.
Don’t restart the infusion until the reaction is fully gone. If it was mild, you can resume later at a slower rate. If it was severe-low blood pressure, chest pain, trouble breathing-then you need to pause vancomycin and consider alternatives.
For patients who’ve had a reaction before and need vancomycin again, premedication may help:
- Diphenhydramine (Benadryl) 25-50 mg IV, 30 minutes before the infusion
- Ranitidine 50 mg IV (or famotidine 20 mg IV) to block H2 receptors
But here’s the key: Don’t premedicate everyone. Only use this for patients with a history of VIR. Giving antihistamines to everyone just because they’re getting vancomycin is unnecessary, adds cost, and causes side effects like drowsiness. It’s not a blanket solution.
What If You Can’t Slow It Down?
Sometimes, speed is necessary. A patient is crashing with sepsis. Time is critical. You need vancomycin now.
In those cases, you can:
- Premedicate with diphenhydramine and famotidine
- Use a central line instead of a peripheral IV-better flow control
- Consider alternative antibiotics if available: linezolid, daptomycin, or ceftaroline
Some hospitals use desensitization protocols for patients with true allergies who absolutely need vancomycin. This involves giving tiny, gradually increasing doses over several hours under close monitoring. It’s complex and only done in controlled settings.
Other Antibiotics That Can Cause Similar Reactions
Vancomycin isn’t the only drug that causes flushing. Others include:
- Amphotericin B: Causes histamine release through complement activation. Often called ‘shake and bake’ because of chills and fever.
- Rifampin: Triggers hypersensitivity by forming reactive metabolites that bind to proteins.
- Ciprofloxacin: Rarely causes flushing, especially if infused too fast.
If you’ve had a reaction to one of these, you might be more prone to others. Always check for a history of similar reactions before starting any new IV antibiotic.
Bottom Line: Slow It Down, Skip the Jargon
Vancomycin infusion reaction is not an allergy. It’s not rare. And it’s not inevitable. It’s a simple, preventable side effect caused by speed-not the drug itself. Slowing the infusion to 10 mg per minute or less stops it in almost every case. No extra drugs needed. No guesswork.
Stop using ‘red man syndrome.’ It’s outdated, inaccurate, and harmful. Use ‘vancomycin infusion reaction’ or ‘vancomycin flushing syndrome’ in all records. That’s not just politically correct-it’s clinically essential.
If you’re a patient, ask: ‘How fast will this be given?’ If you’re a clinician, slow it down. Your patient will thank you.
Is vancomycin infusion reaction the same as an allergy?
No. A vancomycin infusion reaction is not an allergy. It’s an anaphylactoid reaction caused by direct histamine release from mast cells, triggered by rapid infusion. True allergies involve IgE antibodies and require prior exposure. You can have a flushing reaction on your first dose of vancomycin, which wouldn’t happen with a true allergy.
Can vancomycin infusion reaction be fatal?
Rarely. Most reactions are mild-flushing and itching. But in rare cases, rapid infusion can cause severe hypotension or chest pain that mimics a heart attack. If left untreated, low blood pressure can lead to organ stress. That’s why stopping the infusion and monitoring vitals is critical. Death from this reaction alone is extremely uncommon.
Why do some hospitals still use the term ‘red man syndrome’?
Some still use it out of habit or because older records haven’t been updated. But major institutions like UCSF, Harvard, and the Infectious Diseases Society of America have officially moved to ‘vancomycin infusion reaction’ or ‘vancomycin flushing syndrome.’ The 2021 Hospital Pediatrics study showed that after implementing terminology changes, the use of the old term dropped by 17% in just three months. Change is happening, but it’s not universal yet.
Do I need to take Benadryl before every vancomycin dose?
No. Premedication with diphenhydramine is only recommended for patients who’ve had a previous infusion reaction and need vancomycin again. Giving it to everyone adds side effects like drowsiness and doesn’t prevent the reaction if the infusion is too fast. Slowing the infusion is the real solution.
Can I get this reaction from oral vancomycin?
No. Oral vancomycin is not absorbed into the bloodstream. It’s used only for intestinal infections like C. diff. Since it doesn’t enter systemic circulation, it cannot cause infusion reactions. The reaction only happens with intravenous (IV) administration.
How long should a 1,000 mg dose of vancomycin take to infuse?
A 1,000 mg dose should be infused over at least 100 minutes to stay at or below 10 mg per minute. Many hospitals choose 90-120 minutes for added safety. Infusing it faster than 10 mg per minute significantly increases the risk of flushing, itching, and low blood pressure.
Are there alternatives to vancomycin if I’ve had a reaction?
Yes. If you’ve had a severe reaction and can’t safely receive vancomycin, alternatives include linezolid, daptomycin, ceftaroline, or telavancin. The choice depends on the infection type, kidney function, and local resistance patterns. Always consult an infectious disease specialist when switching antibiotics.

2 Comments
vancomycin infusion reaction? more like vanco-slam. stop rushing it. done.
red man syndrome was fine lol why u so mad now