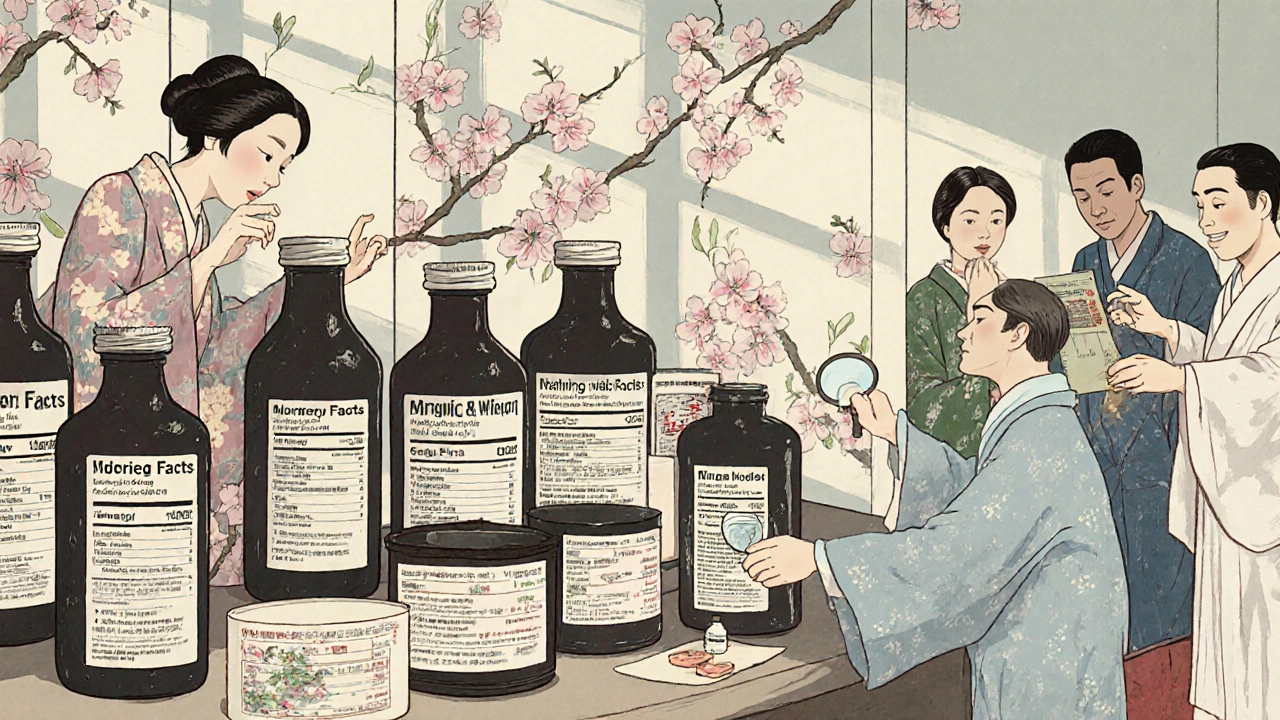
Over-the-Counter Safety: What You Need to Know Before Taking OTC Medicines
When you grab a bottle of over-the-counter safety, the practice of using non-prescription medicines without medical supervision while avoiding harm. Also known as OTC medication use, it's something millions do every day without thinking twice. But just because you don't need a prescription doesn't mean it's harmless. Many people assume OTC means safe, but that’s a dangerous myth. Painkillers like ibuprofen can wreck your stomach or kidneys if taken too long. Cold meds with pseudoephedrine can spike your blood pressure. Even antacids, when used daily for months, can cause nutrient loss or rebound acid production. Over-the-counter safety isn’t about avoiding meds—it’s about using them right.
One of the biggest risks? drug interactions, when two or more medicines react in ways that change their effects, often dangerously. A common cold pill might contain acetaminophen, and if you’re also taking a prescription painkiller with the same ingredient, you could overdose without realizing it. Same goes for herbal supplements. Ashwagandha, turmeric, or even St. John’s Wort can mess with thyroid meds, blood thinners, or antidepressants—something you won’t find on the OTC label. And it’s not just pills. Topical creams with NSAIDs can get absorbed into your bloodstream, especially if you have broken skin or use them over large areas. These aren’t edge cases—they happen daily, often to older adults taking five or more products at once.
OTC side effects, unwanted reactions from medicines taken as directed, often ignored because they seem "normal" are another hidden danger. Drowsiness from antihistamines? Many think it’s just part of the deal. But if you’re driving, operating machinery, or caring for kids, that drowsiness becomes a risk. Constipation from calcium-based antacids? You might chalk it up to diet. But it could be a sign your body’s overwhelmed. And then there’s medication misuse, using a drug in a way not intended, like taking more than directed or for longer than recommended. People take painkillers daily for headaches, sleep aids for anxiety, or laxatives for weight loss—each time, they’re playing Russian roulette with their organs.
What makes this worse is that most OTC labels don’t tell you what you really need to know. They list side effects in tiny print, but not how often they happen, or who’s most at risk. A 70-year-old with kidney issues? Their risk from NSAIDs is way higher than a 25-year-old’s. Someone on blood pressure meds? Decongestants could be a silent threat. You can’t rely on the box—you need to understand what’s inside and how your body reacts to it. That’s why real over-the-counter safety isn’t about being scared of OTCs—it’s about being informed. It’s about asking: Is this right for me? Am I doubling up? Could this mess with something else I take? And when should I just call a doctor instead of reaching for the shelf?
The posts below dive into real cases where OTC use went wrong—and how to avoid it. You’ll find what happens when OTC drugs clash with prescriptions, how to spot hidden ingredients, why "natural" doesn’t mean safe, and what to do when you’ve been taking something for too long. No fluff. Just facts you can use to protect yourself, your family, and your health.
OTC switches let you buy former prescription drugs without a doctor, but they come with hidden risks. Learn how to use them safely, avoid dangerous interactions, and protect yourself from overdose and misdiagnosis.