OTC Medication Risks: What You Need to Know Before Taking Them
When you grab an OTC medication, a drug sold without a prescription, often used for minor symptoms like headaches, allergies, or stomach upset. Also known as non-prescription medicine, it’s easy to assume these are harmless because you don’t need a doctor’s note to buy them. But that’s exactly where the danger starts. Millions of people take OTC medication every day without thinking twice—until something goes wrong. A headache pill combined with a cold remedy causes dizziness. An antacid masks stomach pain that’s actually a heart attack. A sleep aid makes an elderly person fall. These aren’t rare accidents. They’re predictable outcomes of ignoring how these drugs behave in real life.
One major risk is drug interactions, when two or more substances affect each other in harmful ways. You might think taking ibuprofen with your daily aspirin is fine, but together they can wreck your stomach lining or kidneys. Or you pop melatonin for sleep while on a blood thinner—and suddenly you’re bruising easily. Even natural supplements like ashwagandha, a popular herb used for stress and thyroid support, can interfere with thyroid meds or blood pressure drugs. These aren’t theoretical risks. Real cases show up in emergency rooms every week.
Another hidden problem is side effects, unwanted reactions that aren’t always listed clearly on the label. Many OTC drugs carry warnings in tiny print about drowsiness, confusion, or heart rhythm changes—but most people skip them. Seniors are especially vulnerable. A common cough syrup with dextromethorphan can cause hallucinations in older adults. Painkillers like acetaminophen quietly damage the liver if taken too often, especially with alcohol. And let’s not forget the long-term risks: using nasal sprays for months can cause rebound congestion. Taking antacids daily? You might be lowering your magnesium or vitamin B12 without knowing it.
What makes this worse is that people treat OTC drugs like candy. They double up because "it didn’t work fast enough." They mix them with alcohol because "it’s just a little." They keep using them for weeks because "it’s not serious." But the body doesn’t care if a drug is sold over the counter. It reacts the same way to active ingredients, no matter the price tag or packaging. That’s why postmarketing data—real-world reports after a drug hits shelves—shows more harm from OTC meds than most people realize. These aren’t just minor complaints. They’re preventable hospitalizations.
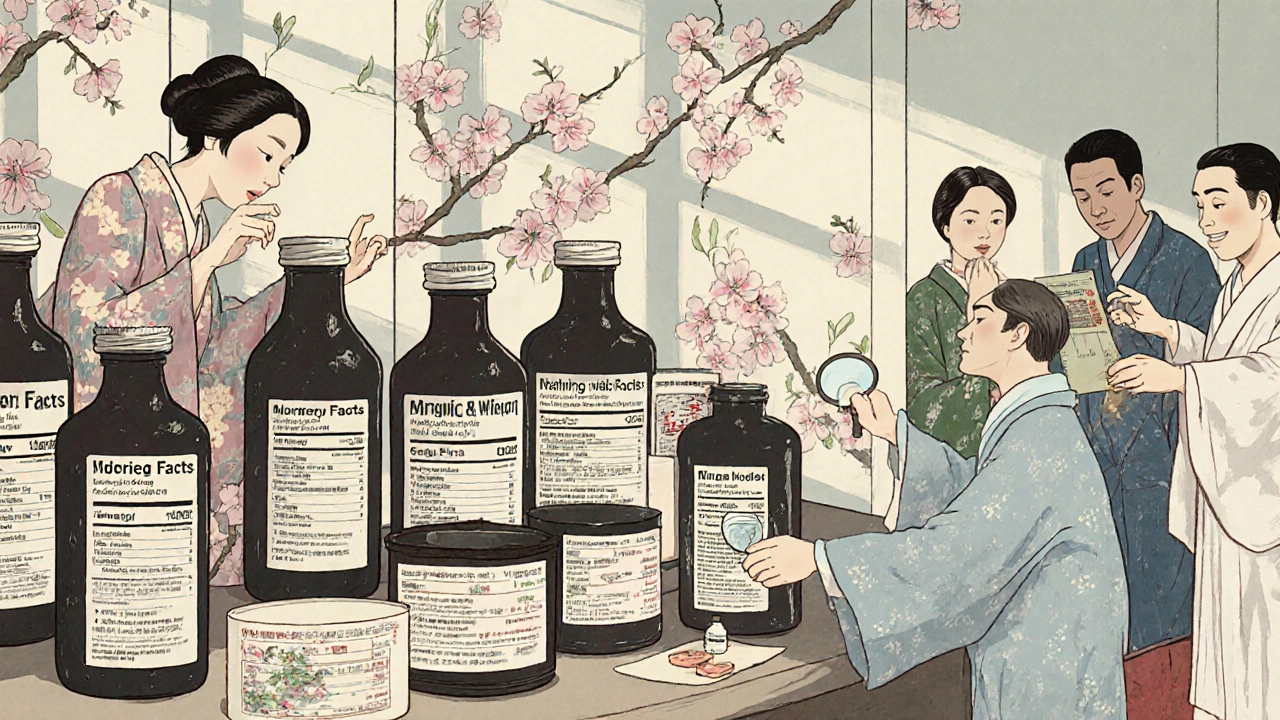
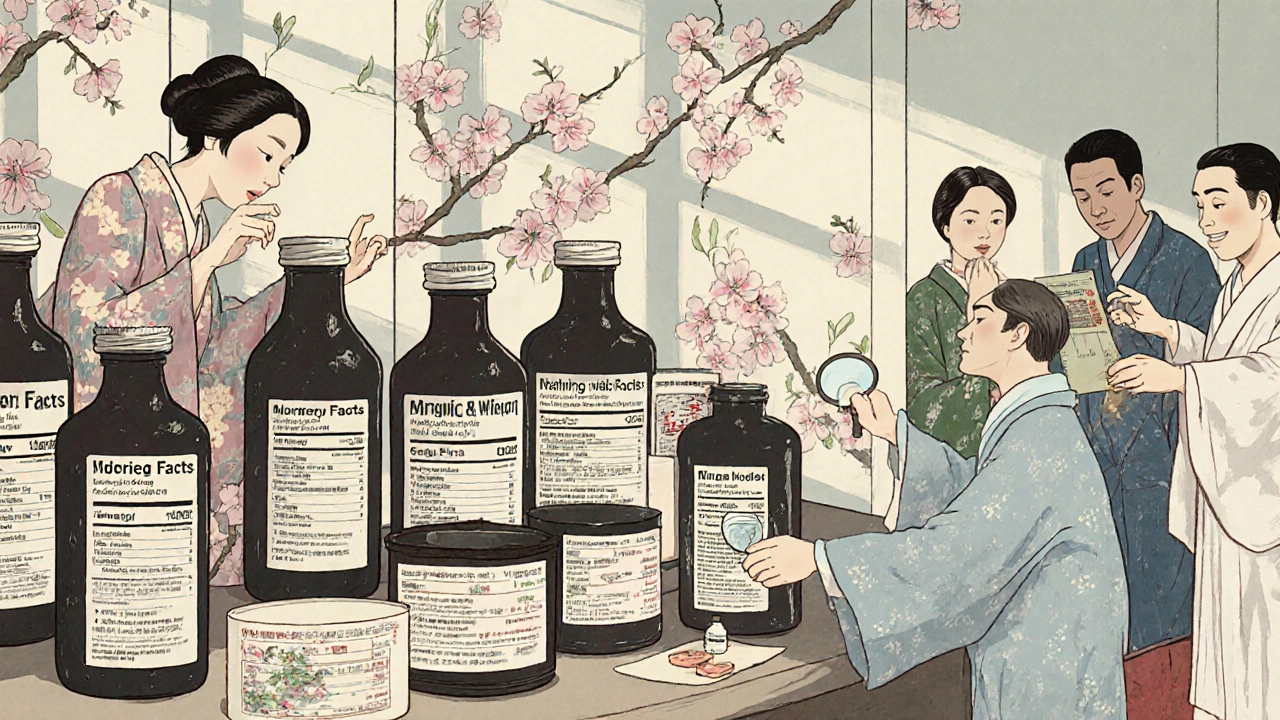
You don’t need to avoid OTC medications. You just need to treat them like real medicine. Check labels for active ingredients. Avoid stacking products with the same drug (like two cold remedies that both contain acetaminophen). Talk to your pharmacist—not just when you buy, but when you’re unsure. And if you’re on other prescriptions, especially for heart, thyroid, or mental health, ask if your OTC choices are safe. The truth is simple: no drug is risk-free. Just because you can buy it without a prescription doesn’t mean you should take it without thinking.
Below, you’ll find real cases, clear comparisons, and practical advice on how to spot danger before it hits. From hidden interactions to long-term damage, these posts break down what most guides leave out—and why knowing this could save your health.
OTC switches let you buy former prescription drugs without a doctor, but they come with hidden risks. Learn how to use them safely, avoid dangerous interactions, and protect yourself from overdose and misdiagnosis.