
Diabetes Sick Day Medication Guide
Sick Day Assessment
Answer these questions to get personalized guidance on medication adjustments during illness.
Hydration & Monitoring
You should aim for at least 1,500 mL of fluids daily. Test glucose every 2-4 hours and check ketones if glucose exceeds 240 mg/dL.
Medication Guidance
When to Seek Emergency Care
When you’re under the weather, the last thing you want is a life‑threatening crisis. Sick Day Rules are a set of evidence‑based steps that tell you how to manage diabetes medicines, fluids, and monitoring when illness strikes. By following these rules you dramatically lower the odds of diabetic ketoacidosis (DKA) and acute kidney injury (AKI), two complications that surge three‑fold during a flu or stomach bug.
Why sick‑day planning matters
Illness puts your body under stress: fever, vomiting, or diarrhea dehydrate you, raise hormone levels, and push blood glucose out of its usual range. A 2022 JAMA Internal Medicine analysis of 47,892 hospital admissions showed a 300 % increase in DKA and a 200 % rise in AKI among people with diabetes during acute illness. In the United States alone, 12.7 % of diabetes‑related hospitalizations stem from medication mishandling on sick days (CDC, 2023). That’s why the American Diabetes Association (ADA) has updated its sick‑day guidance every two years, most recently in January 2023.
Core principles that apply to every diabetes type
- Hydration first: aim for at least 1,500 mL of fluid daily; NICE lowers the threshold to 1,200 mL for high‑risk patients.
- Frequent glucose checks: test every 2-4 hours (minimum six times a day) and keep readings between 100‑180 mg/dL (5.6‑10 mmol/L).
- Ketone vigilance: start urine or blood ketone testing once glucose exceeds 240 mg/dL (13.3 mmol/L).
- Medication review: pause or adjust any drug that can worsen dehydration, lactic acidosis, or ketoacidosis.
Medication‑specific sick‑day rules
Not all diabetes meds behave the same when you’re sick. Below is the most current guidance (ADA 2023, IDF 2022, NICE 2023) for each major class.
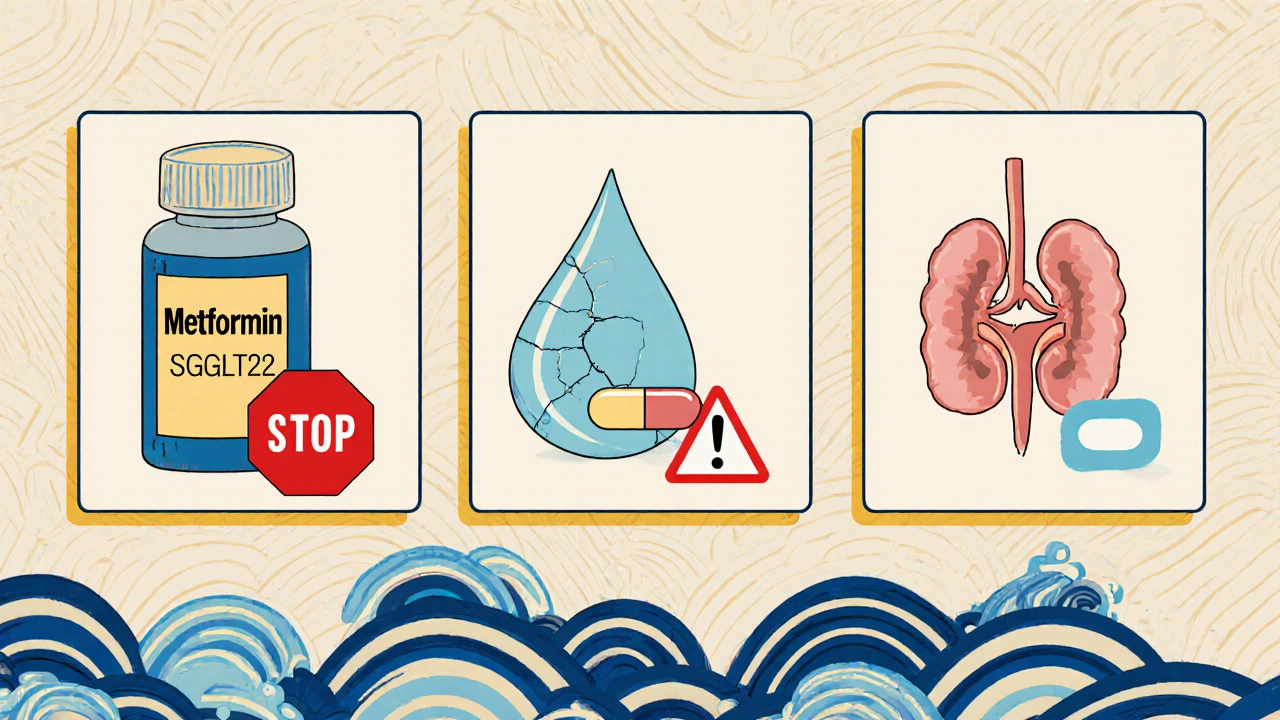
Metformin must be stopped at the first sign of vomiting, diarrhea, or fever because rising creatinine (>1.5 mg/dL) makes lactic acidosis 8.3‑times more likely (NEJM 2019). Restart only after fluid intake is back to normal and a doctor confirms kidney function is stable.
SGLT2 inhibitors (empagliflozin, dapagliflozin, canagliflozin) need immediate discontinuation when you can’t stay hydrated. The FDA’s 2021 safety alert linked these drugs to a 7.2‑fold rise in euglycemic DKA under dehydration.
ACE inhibitors and ARBs (e.g., lisinopril, losartan) should be paused if fluid intake drops below 1,500 mL/24 h. A 2022 meta‑analysis showed a 40 % increase in AKI risk when these agents are kept during low‑volume states.
Sulfonylureas (glipizide, glyburide) can cause dangerous hypoglycemia when food intake falls. Reduce the dose by half or hold the drug until you’re eating regular meals again.
Guidelines for newer agents such as GLP‑1 receptor agonists remain vague; most experts recommend continuing them unless you experience significant nausea or vomiting that prevents any oral intake.
Insulin adjustments on sick days
Insulin needs the most careful tweaking because you’re already dealing with fluctuating glucose.
- Type 1 diabetes: increase basal rates by 10‑20 % every 4 hours if glucose stays >15 mmol/L (270 mg/dL). Keep rapid‑acting insulin on hand for correction doses.
- Type 2 diabetes on insulin: individualize the increase; a 2023 Diabetes Care trial found 68 % of participants needed a dose boost, often 10‑30 % higher than usual.
Always have a “15‑15 rule” ready: 15 g fast‑acting carbs every 15 minutes for a low <70 mg/dL that doesn’t respond to a single dose.
Monitoring: glucose, ketones, and kidney function
During illness, your testing schedule tightens. Use a reliable meter and keep at least 50 test strips on hand. Record each reading in a log (paper or app) and note fluid intake.
Ketone testing thresholds:
- Urine ketones > 1.5 mmol/L or blood ketones > 0.6 mmol/L → call your provider immediately.
- If ketones stay elevated after two hours despite hydration, seek emergency care (risk of DKA).
Watch for early AKI signs: reduced urine output, swelling in ankles, or a sudden rise in serum creatinine (>0.3 mg/dL in 48 h). If you notice any, pause ACE/ARB drugs and contact your clinician.
Build a sick‑day kit before flu season
Preparation is half the battle. Aim to assemble your kit by early October.
- Glucose meter plus at least 50 test strips.
- Ketone testing strips (minimum 10).
- 7‑day supply of all diabetes meds (including backup pens for insulin).
- 7 bottles of 12‑oz sugar‑free beverage (sports drinks, electrolyte packets such as Nuun Hydration).
- Documentation: a printed sick‑day log, emergency phone numbers, and a list of medication adjustments.
- Rapid‑acting carbohydrate source (glucose tablets, fruit juice).
Set alarms on your phone to remind you of the 2‑4 hour glucose checks. The ADA’s online Sick Day Planner (updated quarterly) can be printed and tucked into your kit.
When to call a doctor or go to the ER
Even with a solid plan, some red flags demand professional care:
- Blood glucose <70 mg/dL that doesn’t improve after two 15‑g carbs.
- Persistent ketones >1.5 mmol/L for more than two hours.
- Vomiting longer than 4 hours or diarrhea longer than 6 hours.
- Fluid intake <1,200 mL/24 h despite attempts to drink.
- Signs of AKI: swelling, dark urine, or a rapid rise in creatinine.
The ADA’s 24/7 helpline (1‑800‑DIABETES) answers 92 % of calls within three minutes - keep that number saved.
Common pitfalls and how to avoid them
Patients often stumble over contradictory advice from different providers. A 2024 Endocrine Practice study found 41 % received mixed instructions. To stay on track:
- Ask your primary care doctor and endocrinologist to agree on a single sick‑day protocol.
- Write down which meds to stop, reduce, or keep - don’t rely on memory.
- Review your kidney function baseline before flu season; share the numbers with your care team.
- If you’re over 65 or have multiple comorbidities, involve a pharmacist for medication reconciliation.
Remember the “5‑day rule” quoted by Dr. Robert Gabbay (ADA): restarting a paused medication after more than five days without medical clearance spikes AKI risk by 18 %.
When should I stop my Metformin during illness?
Stop Metformin at the first sign of vomiting, diarrhea, or fever that keeps you from drinking enough fluids. Restart only after you’re hydrated, kidney labs are normal, and a clinician approves.
Do I need to pause my SGLT2 inhibitor even if I only have a mild cough?
Yes. The FDA warns that any reduced fluid intake with SGLT2 inhibitors can trigger euglycemic DKA. If you’re not drinking at least 1,500 mL per day, discontinue the drug until you’re well‑hydrated.
How often should I test my blood sugar on a sick day?
Every 2-4 hours, aiming for at least six readings in 24 hours. If you’re using an insulin pump, check more frequently as instructed by your diabetes team.
What are the warning signs of DKA I should watch for?
Fruity‑smelling breath, nausea, vomiting, abdominal pain, rapid breathing (Kussmaul breaths), and blood glucose >240 mg/dL with rising ketones. Call emergency services immediately if these appear.
Can I keep my ACE inhibitor if I’m only slightly dehydrated?
If fluid intake falls below 1,500 mL/24 h, pause the ACE inhibitor or ARB. Even mild dehydration can tip the balance toward AKI in susceptible patients.
What should I do if my blood sugar stays low despite carbohydrate intake?
Follow the 15‑15 rule: 15 g fast‑acting carbs every 15 minutes until you reach >70 mg/dL. If you can’t raise it, seek medical help right away.

15 Comments
Another day, another endless list of sick‑day rules that read like a textbook for med students. The article drags on with statistics that make me want to curl up in a ball. Yet, the core advice-hydrate, monitor, adjust meds-is undeniably lifesaving. If you’re already drowning in glucose numbers, this could be a lifeline, albeit served on a bland platter. Still, the tone feels like a lecture from a weary professor.
The step‑by‑step checklist makes sick‑day planning feel manageable.
I thnik the article captures the uneasy balance between control and chaos when illness strikes.
It reminds us that mindfulness about fluid intake can be a form of self‑care, not just a medical chore.
Yet, there is a subtle call to trust our bodies while we trust the guidelines.
Embrace the paradox, and you may dodge DKA.
Oh, marvelous-another exhaustive list of what not to do. 🙄 If you enjoy reading legalese disguised as health advice, this is your jam.
Having a clear sick‑day plan is essential for anyone living with diabetes.
First, keep a dedicated kit that includes a glucose meter, enough test strips, and ketone testing supplies.
Second, aim to drink at least 1.5 liters of fluid each day, adjusting upward if you have a fever or vomiting.
Third, check your blood glucose every two to four hours, even if you feel fine.
Fourth, if your readings rise above 240 mg/dL, start testing for ketones immediately.
Fifth, pause medications such as metformin and SGLT2 inhibitors as soon as you notice dehydration or gastrointestinal upset.
Sixth, if you are on insulin, increase basal rates by about 10‑20 % and have rapid‑acting insulin ready for corrections.
Seventh, do not skip meals; if you cannot eat, use the 15‑15 rule with fast‑acting carbs.
Eighth, monitor for signs of acute kidney injury, like reduced urine output or swelling, and hold ACE inhibitors if fluid intake drops.
Ninth, keep a written log of your glucose, ketone levels, fluid intake, and any medication changes.
Tenth, set phone alarms to remind you of the regular glucose checks, especially during the night.
Eleventh, share your sick‑day plan with a trusted family member or caregiver so they can help if you become too ill to manage yourself.
Twelfth, know the red‑flag thresholds that require medical attention, such as glucose below 70 mg/dL despite carbs or persistent vomiting for more than four hours.
Thirteenth, keep emergency contact numbers and a copy of your medication list in an easily accessible place.
Finally, revisit and update your plan each season, because guidelines evolve and your personal needs may change.
Skipping metformin at the first sign of nausea is non‑negotiable. 🚫💊 Ignoring this puts you at risk for lactic acidosis.
The article commendably synthesizes multiple guideline updates, yet its prose could benefit from a more concise structure. By truncating redundancies, the salient points would emerge with greater clarity. Nonetheless, the inclusion of concrete fluid targets is a valuable addition.
Don’t wait for a crisis-prepare your sick‑day kit now! Your future self will thank you when the flu hits.
If you notice swelling in your ankles, stop ACE inhibitors and call your doctor.
Only a fool would think hydration is optional during illness; the body’s demand for water skyrockets as cortisol surges. Dehydration fuels both DKA and AKI, creating a perfect storm that can overwhelm even seasoned clinicians. Trust the science and drink aggressively.
Ah yes, because the average patient has time to parse nuanced pharmacologic adjustments amidst a cough and fever.
Who needs a checklist when you can wing it? The chaos itself is the best teacher, after all.
I find the steadfast insistence on halting ACE inhibitors at 1,500 mL fluid intake both prudent and pedantic. While some may balk at such precision, the data on AKI risk is undeniable. Yet, remember that medicine is an art as much as a science; individual tolerance can vary. Engage your physician rather than following a rulebook blindly.
If you’re unsure about adjusting insulin, reach out to your diabetes educator-they can guide you through the changes safely.
Keeping a calm mindset can make the sick‑day plan easier to follow.
Rise above the weakness of illness and dominate your glucose levels! Your determination today prevents a hospital visit tomorrow.