
Why PSA Screening Is So Controversial
Every year, millions of men get a simple blood test called PSA to check for prostate cancer. It’s quick, cheap, and widely available. But here’s the problem: for every life it saves, it can trigger a chain reaction of biopsies, anxiety, and treatments that don’t actually help - and sometimes make things worse.
The test measures prostate-specific antigen, a protein made by the prostate gland. A high level can mean cancer. But it can also mean a swollen prostate, an infection, even riding a bike the day before. About 75% of men with PSA levels between 4 and 10 ng/mL don’t have cancer at all. And yet, they’re often sent for a biopsy - a painful, risky procedure that can cause bleeding, infection, or hospitalization.
On the flip side, 15% of men with aggressive, life-threatening prostate cancer have PSA levels below 4.0 ng/mL. That means the test misses some of the worst cases. It’s not a perfect tool. It’s not even a good one by modern standards. But it’s the one we’ve been using for decades.
What the Studies Actually Show
Two massive studies, one in Europe and one in the U.S., looked at over 600,000 men over ten years. The European study found PSA screening cut prostate cancer deaths by 21%. The American study found no benefit at all. Why the difference? In the U.S., many men in the "no screening" group still got tested anyway. That blurred the results.
But even in the European study, the benefit came at a heavy cost. For every 1,000 men screened every year for 10 years:
- 1 to 2 deaths from prostate cancer were prevented
- 100 to 120 men had false positives and went through unnecessary biopsies
- 80 to 100 men were diagnosed with cancers that would never have caused symptoms or shortened their lives
These are the cancers that doctors call "indolent" - slow-growing, harmless tumors. But once found, they’re often treated with surgery or radiation. And those treatments? They can cause permanent incontinence, erectile dysfunction, bowel problems. Men wake up after surgery thinking they’ve beaten cancer - only to realize they’ve traded one problem for two worse ones.
Shared Decision-Making Isn’t Just a Buzzword - It’s the Only Ethical Way Forward
The U.S. Preventive Services Task Force changed its recommendation in 2018. No longer saying "don’t screen." Now saying: "If you’re a man between 55 and 69, talk to your doctor before deciding." That’s shared decision-making. And it’s not optional anymore. It’s the standard.
But here’s the catch: most doctors don’t do it well. A 2022 study found primary care doctors spend an average of just 3.7 minutes discussing PSA screening. That’s less time than it takes to check your blood pressure. Meanwhile, experts say you need 15 to 20 minutes to properly explain the trade-offs.
What should that conversation include?
- That PSA screening might reduce your chance of dying from prostate cancer by about 1 in 1,000 over 10 years
- That you’re more likely to be harmed by the test than helped - with unnecessary biopsies, anxiety, or treatment you don’t need
- That if you’re diagnosed, you might not need treatment right away - active surveillance is now a safe, proven option for low-risk cases
- That your race matters - Black men have a 70% higher risk of prostate cancer and are more likely to die from it
- That if your PSA is below 1.0 ng/mL at age 45, you may never need another test
Yet only 60% of men report ever hearing any of this. Too often, the conversation goes: "You’re due for your PSA test." Not: "Here’s what it might do to you. Here’s what it might not do. Let’s decide together."
What’s Replacing PSA? The New Tools (And Why They’re Not a Magic Fix)
There are better tests out there - but they’re not perfect, and they’re not cheap.
MP-MRI scans can show suspicious areas in the prostate before a biopsy. The PRECISION trial found using MRI first cut unnecessary biopsies by 27%. But an MRI costs $400 to $600. Not everyone can get one. And even MRI can miss some cancers.
The 4Kscore test looks at four different proteins in the blood. It’s 95% good at spotting men who won’t have aggressive cancer. But it costs $400 to $600. Most insurance won’t cover it unless you’re already in a high-risk group.
Then there’s the new IsoPSA test - approved by the FDA in 2021. It claims to be 92% accurate at finding high-grade cancer, compared to just 25% for traditional PSA. That’s a big leap. But it’s still new. Not widely available. And still not perfect.
AI is coming too. MIT researchers built an algorithm that predicts prostate cancer risk from routine blood tests. It’s 85% accurate and could cut unnecessary PSA tests by 30%. But it’s still in trials. Not in clinics yet.
So here’s the reality: PSA is still the most common first step. Because it’s cheap. Because it’s everywhere. Because we don’t have a better, affordable, widely available alternative - yet.
What Happens When Men Skip PSA Screening?
Since 2010, PSA screening rates in the U.S. have dropped from 42% to 29% among men 55 to 69. That’s a 31% decline.
And guess what happened? The number of men diagnosed with metastatic prostate cancer - cancer that’s already spread beyond the prostate - jumped by 37% between 2004 and 2013. That’s not a coincidence. It’s a consequence.
Some of those men are dying from cancers that could have been caught early. One man in his 60s, diagnosed with stage 4 cancer after skipping screening for years, told his story on a prostate cancer forum: "I thought I was fine. I didn’t have symptoms. Now I’m on chemotherapy. If I’d known, I’d have gotten tested."
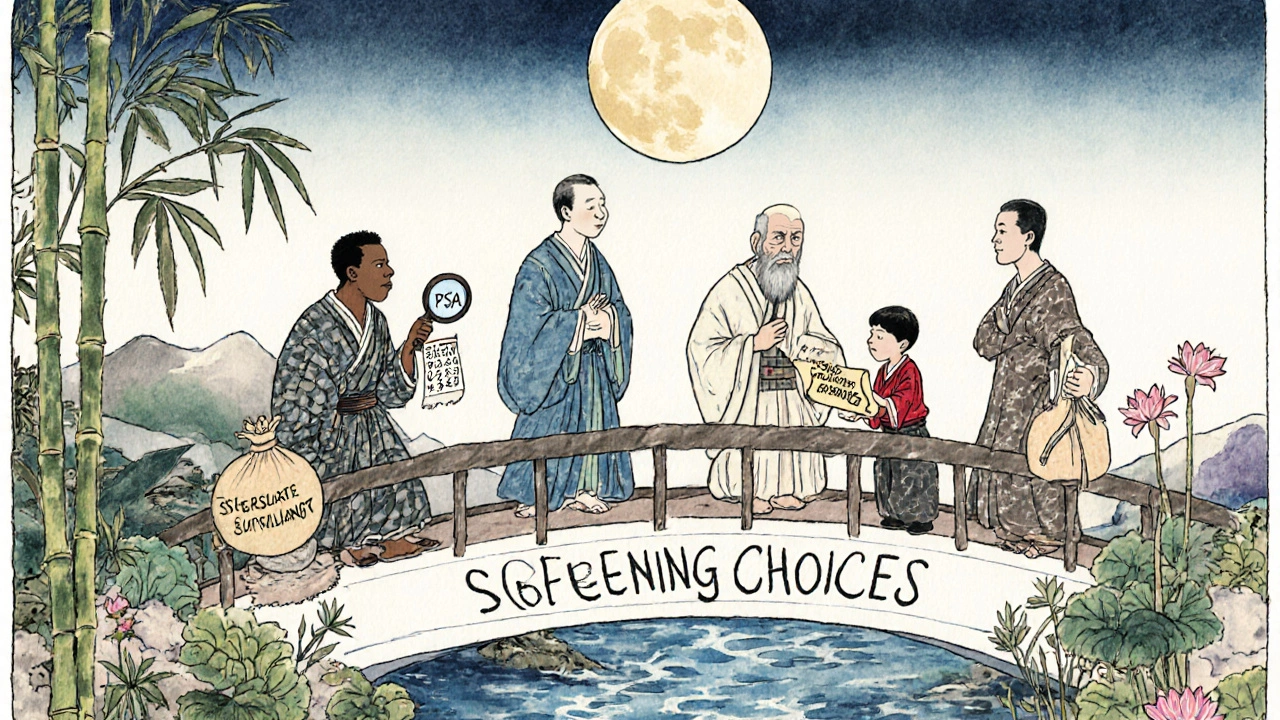
Who Should Get Tested? And Who Should Skip It?
There’s no one-size-fits-all answer. But here’s what the evidence says:
- Men 55 to 69: This is the group where screening has the best chance of helping. But only if you understand the risks. Talk to your doctor.
- Men under 55: Only if you’re Black, or have a father or brother who got prostate cancer before 65. Even then, start with a baseline PSA at 45.
- Men 70 and older: The U.S. Preventive Services Task Force says the harms outweigh the benefits. If you’re healthy and active, talk to your doctor. But for most, screening is not recommended.
- Men with PSA under 1.0 ng/mL at age 45: You’re at very low risk. You may never need another test.
- Men with PSA above 3.0 ng/mL at age 50: You’re at higher risk. You need more frequent checks and possibly an MRI.
And if you’re Black? You’re more likely to get prostate cancer. More likely to die from it. Yet you’re 23% less likely to get a proper shared decision-making conversation. That’s not just a gap in care - it’s a systemic failure.
What to Do Next
If you’re a man between 55 and 69:
- Ask your doctor: "Have we talked about the pros and cons of PSA screening?" If not, say: "I want to make an informed choice. Can we go over the risks and benefits?"
- Ask: "What’s my baseline PSA? What’s my risk based on my race, family history, and age?"
- Ask: "If my PSA is high, what happens next? Do I automatically get a biopsy? Or can we do an MRI first?"
- Ask: "If I’m diagnosed, what are my options besides surgery or radiation? Is active surveillance right for me?"
- Ask: "Can I get a decision aid - something visual - to help me understand the numbers?"
Don’t let fear or inertia make the decision for you. Don’t let a 3-minute appointment decide your future. This isn’t about whether PSA is good or bad. It’s about whether you’re making a choice - or just letting someone else make it for you.
What If You’ve Already Been Diagnosed?
Many men panic when they hear "prostate cancer." But here’s the truth: not all prostate cancers need to be treated right away. In fact, most don’t.
Active surveillance means regular PSA tests, MRIs, and occasional biopsies - not surgery. The ProtecT trial showed that after 10 years, survival rates were identical between men who had surgery, radiation, or just watched. No difference in death rates. But big differences in side effects.
If you’ve been diagnosed with low-risk cancer, ask: "Is active surveillance an option?" If your doctor doesn’t mention it, ask again. You have time. You don’t need to rush into treatment.
Is PSA screening still recommended?
Yes - but only after a shared decision-making conversation with your doctor. The U.S. Preventive Services Task Force recommends PSA screening for men aged 55 to 69, but only if they understand the risks and benefits. It’s no longer a routine test - it’s a personal choice.
Does PSA screening save lives?
It can - but rarely. For every 1,000 men screened over 10 years, only 1 to 2 prostate cancer deaths are prevented. But for every 1,000 men screened, 80 to 100 are diagnosed with cancers that would never have caused harm. That’s why the debate continues: the benefit is small, and the harm is common.
What’s the biggest risk of PSA screening?
The biggest risk is overtreatment. Many men get biopsies, surgeries, or radiation for cancers that are slow-growing and harmless. These treatments often cause permanent side effects like incontinence and impotence - problems that can last a lifetime. You might "beat" cancer only to lose your quality of life.
Should Black men get PSA screening?
Yes - and they should start earlier. Black men have a 70% higher risk of prostate cancer and more than double the death rate compared to white men. They’re also less likely to get proper counseling before testing. If you’re Black and over 45, talk to your doctor about baseline PSA and risk factors.
Can I avoid PSA screening altogether?
You can - but you should do it with eyes wide open. Skipping screening means you might miss a fast-growing cancer. Between 2004 and 2013, metastatic prostate cancer diagnoses rose 37% as screening rates fell. If you choose not to be screened, make sure you know the signs: trouble urinating, blood in urine or semen, bone pain. Report them immediately.
What’s the best alternative to PSA screening?
There isn’t one yet. MP-MRI and newer blood tests like 4Kscore and IsoPSA are better at finding aggressive cancer, but they’re expensive and not widely used. For now, PSA is still the first step - but it should never be the last. Always follow up with MRI, risk calculators, or genetic tests if your PSA is high.

8 Comments
PSA is a garbage test. 75% false positives? And you call that medicine? It's like using a Magic 8-Ball to diagnose diabetes. Biopsies for nothing, then you get surgery that leaves you incontinent. Brilliant. Just brilliant.
yo so like i read this whole thing and honestly? PSA is just a relic. like why are we still using something from the 90s? i got my 4Kscore done last year for $500 and it was way better. my doc was like 'uhhh we dont usually do this' like duh because its expensive and insurance hates you. but at least i know i dont have the aggressive kind. psa? nah. i dont trust it.
I really appreciate this breakdown. So many guys just get the test because their doctor says 'it's routine' without ever explaining what it actually means. I talked to mine for 20 minutes last month-asked about active surveillance, my family history, even my race-and he actually listened. It felt like the first time I was treated like a person, not a checkbox. If you're 55-69 and haven't had this convo yet? Do it. It's not about fear. It's about ownership.
I just want to say I cried reading this because my dad died of prostate cancer at 67 and he never got tested because he thought he was fine until he started bleeding and then it was too late and now I’m terrified for all the men in my life and also mad at the system that lets doctors rush through this and also why does no one talk about how Black men get screwed over in this system like why is this still happening in 2025
I know this is a heavy topic but I just want to say that I think the most important thing here is that men need to feel like they have the right to ask questions and not feel stupid for not knowing. I’m a woman and I didn’t even know what PSA stood for until my husband got tested last year and then I had to google it and read all this stuff and now I’m like wow this is so complicated and no one ever told us. I think doctors need to give out little pamphlets or videos or something because most guys just say yes to the test because they don’t want to seem weak or like they’re questioning their doctor and that’s not fair. We need better communication not just better tests.
This is the kind of info that should be mandatory in every doctor's office. Not a 3-minute script. A real conversation. I’m 62, had a PSA of 4.2 last year, got an MRI instead of a biopsy, turned out to be benign. No trauma. No incontinence. Just peace of mind. If you’re reading this and you’re in the 55-69 range-don’t wait. Ask for the MRI. Ask for the 4Kscore. Ask for time. You deserve it.
why do americans always make everything so complicated? in india we just get the test and if its high we go to doctor. no 20 min talks no mri no 4kscore. just test and go. sometimes simple is better. also why are you all so scared of cancer? its just a disease. if you die you die. why waste money on all this tech? my uncle had prostate cancer at 70 and lived to 85 without treatment. he just ate mangoes and prayed. maybe you dont need all this fancy stuff.
Thank you for highlighting the racial disparity in care. My brother is Black and was told by his doctor 'PSA isn’t necessary unless you have symptoms'-which is exactly the opposite of what the guidelines say. He finally got a second opinion after his PSA was 6.8 and found out he had a high-risk tumor. He’s on active surveillance now. But if he hadn’t pushed? He’d be in chemo right now. This isn’t just about medicine. It’s about equity. If you’re Black and over 45, don’t wait. Don’t trust silence. Ask. Push. Demand the conversation.