
Millions of people take statins every year to lower their cholesterol and protect their heart. But for a lot of them, the price feels too high: constant muscle aches, soreness, or weakness that makes walking, climbing stairs, or even getting out of bed a struggle. If you’ve been told your pain is "just in your head" or dismissed as "normal," you’re not alone. The truth is, statin-related muscle pain is real - but it’s also often misunderstood. And knowing the difference between a harmless nuisance and a dangerous red flag can make all the difference.
How Common Is Statin Muscle Pain?
Doctors will tell you muscle pain from statins affects less than 5% of users. But if you’ve talked to other patients, you’ve probably heard a very different story. In real life, up to 30% of people on statins report muscle discomfort. Why the gap? Part of it comes down to how studies are done. Clinical trials often exclude older adults, people with other health problems, or those already taking other meds - the very people most likely to feel side effects.
What’s more, the nocebo effect plays a big role. If you’ve read the pamphlet that says "muscle pain is possible," you’re far more likely to notice every little twinge and blame it on the pill. One study found patients who were warned about muscle side effects were 40% more likely to report pain - even if they were taking a sugar pill. That doesn’t mean the pain isn’t real. It just means your brain can amplify it.
What Does Statin Muscle Pain Actually Feel Like?
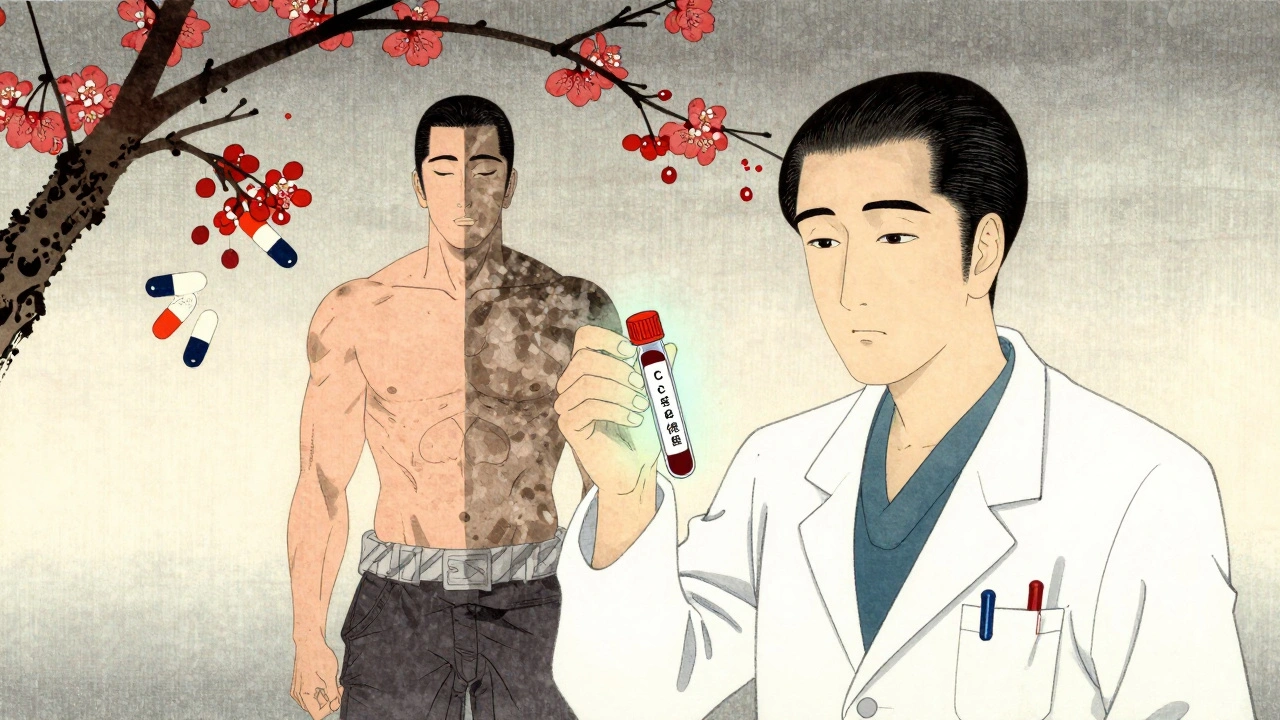
It’s not just soreness after a workout. Statin-related muscle pain usually shows up as a dull, constant ache - not sharp or sudden. It tends to hit both sides of your body equally. Common spots include your thighs, shoulders, hips, and calves. You might feel weak, tired, or just generally "off." Some people say it feels like their muscles are "bruised" from the inside.
Most of the time, it’s mild - what doctors call myalgia. But there’s a spectrum. In rare cases, it can turn into myositis (inflammation) or even rhabdomyolysis - a serious condition where muscle tissue breaks down and floods your bloodstream with toxins. This is extremely rare: about 3 to 5 cases per million prescriptions. But if you notice dark, tea-colored urine, extreme weakness, or swelling in your limbs, get help right away. That’s not something to wait out.
Who’s Most at Risk?
Not everyone on statins gets muscle pain. But some people are far more likely to. Here’s who:
- Women - especially those over 65 or with smaller body frames (under 100 lbs)
- People over 80
- Those with thyroid problems, kidney disease, or liver issues
- People taking other meds like fibrates, certain antibiotics (like erythromycin), or cyclosporine
- Anyone on high-dose statins (like 80 mg of atorvastatin or 40 mg of rosuvastatin)
Hypothyroidism is a big one. If your thyroid isn’t working right, your body handles statins differently - and muscle pain becomes much more likely. Many doctors skip checking thyroid levels before starting statins. That’s a mistake. Fixing your thyroid can make the muscle pain vanish - even if you stay on the statin.
What Should You Do If You Have Muscle Pain?
Don’t stop your statin cold. Stopping without medical advice can raise your risk of heart attack or stroke by 25-50% over the next two years. But you also shouldn’t just push through pain that’s getting worse.
Here’s what actually works:
- Call your doctor. Don’t wait. Mention the pain, where it is, how long it’s been going on, and whether it’s getting worse.
- Get a blood test for creatine kinase (CK). This measures muscle damage. If your CK is more than 10 times the normal level, you need to stop the statin immediately. If it’s only slightly elevated, your doctor might suggest a "statin holiday" - stopping for 4 to 6 weeks to see if symptoms clear up.
- Try switching statins. Not all statins are the same. Pravastatin and fluvastatin are less likely to cause muscle pain than atorvastatin or rosuvastatin. Many people find relief just by switching to a different one.
- Lower the dose. Sometimes, cutting the dose in half (like going from 40 mg to 20 mg of atorvastatin) reduces pain without losing heart protection.
- Check your thyroid. If you haven’t had a TSH test in the last year, ask for one. Untreated hypothyroidism is a hidden trigger.
What About CoQ10 Supplements?
You’ve probably seen ads for Coenzyme Q10 as a fix for statin muscle pain. The theory is that statins lower CoQ10 levels, which your muscles need for energy. Sounds logical - but the science doesn’t back it up.
A major review in the Journal of the American College of Cardiology found no real benefit over placebo. Some small studies showed a drop in pain for a few people, but nothing consistent. If you want to try it, fine - it’s generally safe. But don’t expect miracles. And don’t use it as a reason to keep taking a statin that’s making you miserable.
What Are the Alternatives?
If you’ve tried everything and still can’t tolerate statins, there are other options - but they’re not perfect.
- Ezetimibe: A pill that blocks cholesterol absorption in your gut. It lowers LDL by about 15-20%. It’s cheap (often under $10 a month), and muscle pain is rare.
- PCSK9 inhibitors (alirocumab, evolocumab): These are injectables that can drop LDL by 50-60%. They’re very effective, but cost around $5,000 a year. Most insurance requires you to fail statins first.
- Lifestyle changes: Diet, exercise, weight loss - they all help. But for most people with high cholesterol and heart risk, lifestyle alone isn’t enough. Don’t rely on them as a full replacement unless your doctor says it’s safe.
The key is this: You don’t have to choose between pain and heart attack. There’s a middle ground. It just takes patience and the right strategy.

Can You Ever Get Back on Statins?
Yes - and many people do. A 2018 study found that only 20-25% of people who blamed their muscle pain on statins actually had it return when they tried the same drug again under controlled conditions. That means most of the time, something else was going on: a virus, a new workout, low vitamin D, or even stress.
Doctors often recommend a "rechallenge" - restarting the statin at a lower dose after a break. If the pain comes back, you know it’s the drug. If it doesn’t, you might be able to stay on it long-term. Many patients who thought they couldn’t tolerate statins end up finding a version that works.
What’s the Bottom Line?
Statins save lives. For people with heart disease, diabetes, or high risk, they cut heart attacks and strokes by up to a third. But muscle pain is real, common, and often mishandled.
Don’t assume your pain is "all in your head." Don’t assume you have to suffer to stay healthy. And don’t quit without talking to your doctor.
The goal isn’t to avoid statins at all costs. It’s to find the version, dose, and plan that lets you live without pain - and stay protected from heart disease. That’s possible for most people. You just need to work with your doctor, not against them.
Can statin muscle pain go away on its own?
Yes, in many cases. Muscle pain from statins often improves after stopping the medication for 4 to 6 weeks. For some, switching to a different statin or lowering the dose helps. But if the pain returns when you restart the same drug, it’s likely caused by the statin. Never stop or restart without medical advice.
Is muscle pain from statins a sign of heart problems?
No. Statin-related muscle pain affects your muscles, not your heart. In fact, the statin is helping your heart by lowering cholesterol. But ignoring severe muscle pain could lead to rhabdomyolysis, which can damage your kidneys. That’s why checking creatine kinase levels is important - it tells your doctor if your muscles are breaking down dangerously.
Why do women report statin muscle pain more than men?
Women are more likely to be older when starting statins, have smaller body size, and are more likely to have undiagnosed hypothyroidism - all of which increase risk. They also tend to report symptoms more openly. Some studies suggest hormones may play a role, but the exact reason isn’t fully understood.
Can I take statins every other day to avoid muscle pain?
Some people do, and research is looking into it. The 2023 STRENGTH trial is testing intermittent dosing. Early results suggest it may reduce muscle pain by 40% while still lowering cholesterol. But this isn’t standard advice yet. Only try this under your doctor’s supervision - skipping doses without guidance can reduce heart protection.
Are natural remedies like turmeric or garlic effective for statin muscle pain?
No. While turmeric and garlic may have mild heart benefits, there’s no evidence they reduce statin-related muscle pain. Some supplements can even interfere with how statins are processed by your liver, making side effects worse. Always talk to your doctor before adding anything new to your routine.
How long does it take for muscle pain to go away after stopping statins?
Most people notice improvement within 2 to 4 weeks. For some, it takes up to 6 weeks. If pain persists longer than that after stopping, the cause is likely something else - like arthritis, nerve issues, or vitamin D deficiency. Your doctor can help figure out what’s really going on.
What to Do Next
If you’re experiencing muscle pain and you’re on a statin, your next step is simple: make an appointment with your doctor. Bring a list of your symptoms - when they started, where they hurt, how bad they are on a scale of 1 to 10, and whether anything makes them better or worse.
Ask about your CK levels. Ask if switching statins is an option. Ask about your thyroid. Ask about ezetimibe. Don’t accept "it’s just aging" or "you’re imagining it." You deserve a plan that keeps you safe - without making you miserable.
Statins aren’t the enemy. But ignoring your body’s signals isn’t bravery - it’s risky. The right approach isn’t about choosing between pain and heart disease. It’s about finding the balance that lets you live well - for years to come.

8 Comments
I’ve been on atorvastatin for five years and only realized last year that my constant thigh ache wasn’t just aging. I dropped the dose from 40mg to 20mg and switched to pravastatin. The difference was night and day. No more walking like I’d run a marathon just to the fridge. I wish my doctor had suggested that sooner.
It’s fascinating how the nocebo effect skews perception so dramatically. I work in clinical research, and I’ve seen patients report side effects from placebos simply because they were warned. That doesn’t invalidate their experience-it just means we need better communication. Statins are lifesavers, but we need to frame risks without inducing fear.
CoQ10 is a scam marketed to desperate people. If you’re taking statins and your muscles hurt, you’re either not following diet guidelines or you have an undiagnosed thyroid issue. Stop wasting money on supplements and fix the real problem. Your doctor isn’t lying-you’re just avoiding responsibility.
Thyroid check first. Always.
Whoa-hold on! I’m from India, and here, people are told statins are poison! My uncle had muscle pain, stopped them cold, and now he’s got plaque in his arteries like a road map! This article is a miracle! Why isn’t the WHO screaming about this?! Why are doctors still ignoring thyroid levels?! This is systemic negligence! Someone needs to sue the pharmaceutical industry!
It is imperative to underscore that the pharmacokinetic interplay between statins and concomitant medications, particularly those metabolized via the CYP3A4 pathway, constitutes a clinically significant pharmacodynamic interaction. Furthermore, the presence of subclinical hypothyroidism, often overlooked in primary care settings, exerts a profound modulatory influence on statin tolerance. It is therefore not merely advisable, but obligatory, to conduct a comprehensive endocrine panel prior to initiating statin therapy, as failure to do so may precipitate iatrogenic myopathy.
Okay, but let’s talk about the *aesthetic* of this whole thing-like, imagine your muscles feeling like they’ve been bruised from the inside? That’s not just pain, that’s poetic suffering. And CoQ10? Honey, it’s not a cure, it’s a vibe. A very expensive, slightly hippie vibe. I tried it. Didn’t help. But my Instagram story looked *so* clean with the little blue bottle next to my avocado toast.
I think the real issue isn’t just the drug-it’s how we’ve turned medicine into a binary choice: either you’re fully compliant and suffer, or you’re rebellious and at risk. But what if the middle path is the real healing? Slowing down, listening, switching, testing thyroid, trying ezetimibe… it’s not about being perfect. It’s about being curious. My mom went from hating statins to thriving on 10mg of pravastatin after a thyroid fix. She calls it her quiet victory.