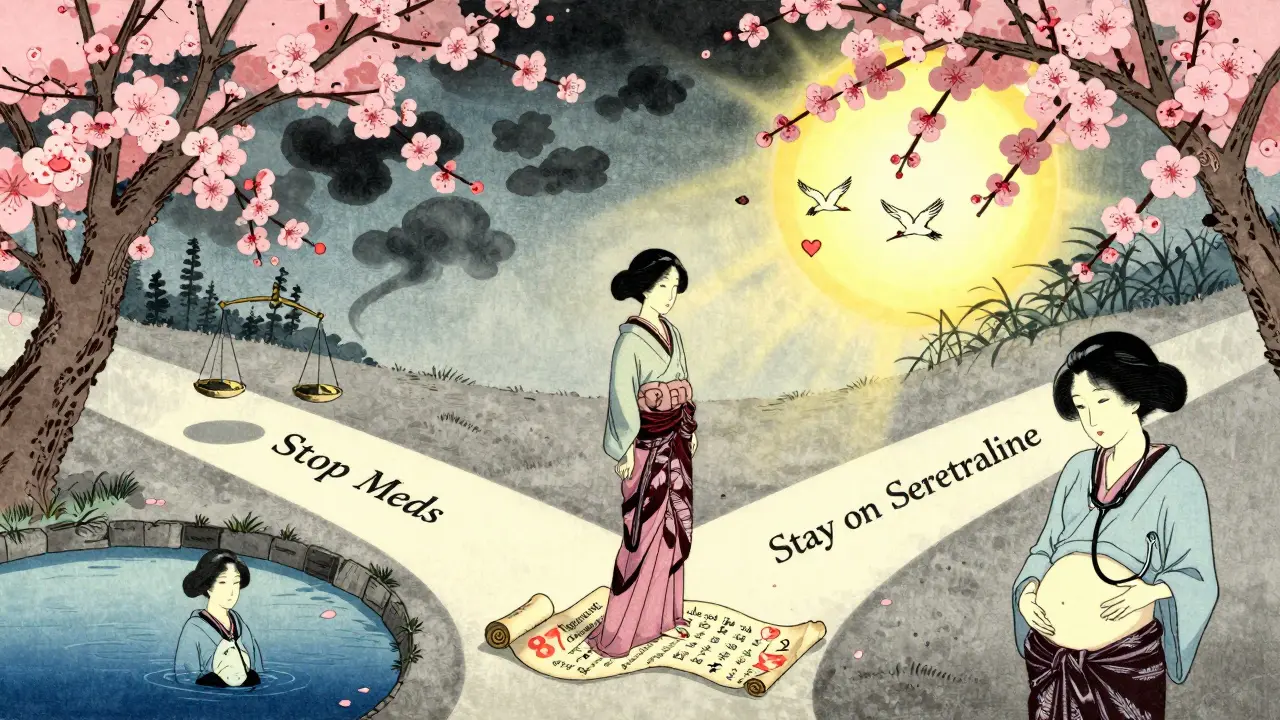
When you’re pregnant and struggling with depression, anxiety, or bipolar disorder, the question isn’t just whether to take medication-it’s how to decide. There’s no easy answer. Stopping your meds might feel safer, but untreated illness carries real risks too. That’s why shared decision-making isn’t just a buzzword-it’s the only way forward.
There’s No Risk-Free Choice
You’ve probably heard that some antidepressants might cause birth defects. That’s true for one: paroxetine. It’s linked to a slightly higher chance of heart problems when taken in the first trimester-rising from about 8 in every 1,000 births to 10 in 1,000. But here’s what most people don’t tell you: untreated depression increases the risk of preterm birth by 30 to 50%. The chance of suicide during pregnancy or after birth goes up by 20% if symptoms aren’t managed. The truth? There’s no perfect option. The goal isn’t to avoid all risk-it’s to choose the least harmful path for you. That’s why doctors now say: Don’t stop your meds without talking to your care team. Many women stop because they’re scared, but 42% of those who quit without guidance end up worse off-some even hospitalized.What Medications Are Safer?
Not all mental health meds are created equal. For depression and anxiety, SSRIs are the first-line choice. Sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac) have the most data backing them. Studies show no major increase in birth defects with these, except for paroxetine. Even then, the added risk is small. For bipolar disorder, lamotrigine is the go-to. It doesn’t raise the risk of major birth defects. Lithium works too, but your body changes during pregnancy-your kidneys process it faster, so your dose needs constant tweaking. Valproic acid? Avoid it. It can double or even triple the risk of neural tube defects like spina bifida. That’s why guidelines now say it shouldn’t be used in anyone who could get pregnant. Bupropion (Wellbutrin) has a small link to miscarriage and heart issues. Tricyclics like nortriptyline are options if SSRIs don’t work, but they’re not first-choice. For psychosis, older antipsychotics like haloperidol and chlorpromazine have decades of safety data. Newer ones? Not enough long-term info on kids exposed in the womb. So unless absolutely necessary, they’re avoided.Shared Decision-Making Isn’t Just a Chat
This isn’t about your doctor telling you what to do. It’s a back-and-forth. Good providers use tools like the Mental Health Medication Decision Aid from ACOG. It breaks down risks in plain numbers: ‘For every 1,000 babies born to moms taking sertraline, 15 may be smaller than average. For paroxetine, 10 may have a heart defect.’ Numbers like that make it real. They also look at your history. If you’ve had two major depressive episodes before, your chance of relapse during pregnancy is 80% if you stop meds. If you’ve been stable for three months before getting pregnant, that risk drops by 40%. That’s not just a statistic-it’s a timeline to plan around. You should walk out of that appointment with:- A clear idea of your personal relapse risk
- Exact numbers on medication risks-not vague warnings
- A plan for what to do if symptoms get worse

What Women Are Really Saying
On Reddit’s r/PostpartumDepression, 125,000 people share their stories. In a recent analysis of 1,243 posts, 78% said they felt pressured to stop their meds. Many did-and 63% ended up needing emergency care. One woman wrote: ‘I stopped Zoloft because my OB said it was ‘unsafe.’ I had a panic attack so bad I called 999. I didn’t know I could’ve stayed on it.’ Meanwhile, women who used structured shared decision-making tools-like the Maternal Outcomes Reflecting Treatment Intensities Scale-were 3.2 times more likely to stick with their treatment plan. At six weeks postpartum, their depression scores were 37% lower. That’s not luck. That’s the power of being heard.What’s New in 2026
The National Pregnancy Registry for Psychiatric Medications has tracked over 15,700 pregnancies since 2010. In 2024, they’re adding newer drugs like brexpiprazole to the list-because we still don’t know enough. But here’s the exciting part: researchers are building tools that don’t just give population averages anymore. A pilot study at Massachusetts General Hospital used machine learning to predict how individual women would respond to meds based on age, weight, past episodes, and genetics. It got 82% of predictions right. By 2026, you might walk into your appointment and see: ‘Of 87 women like you-32, pregnant, history of 3 episodes, on sertraline-only 3 relapsed. Two had babies with minor heart murmurs that fixed themselves.’ That’s not science fiction. That’s where the data is heading.What You Can Do Now
If you’re thinking about getting pregnant-or already are-here’s what to do:- Don’t stop your meds on your own. Even if you feel better, your brain might not be stable yet.
- Ask your provider: ‘What’s my risk of relapse if I stop?’ and ‘What’s the actual risk of this medication?’ Demand numbers, not fear.
- Request the ACOG Decision Aid. It’s free, updated quarterly, and used by most UK and US perinatal clinics.
- Find a perinatal psychiatrist. 87% of obstetricians now consult them before prescribing. You deserve that level of care.
- Write down your decision. What you chose, why, and what you’ll do if things change. Keep a copy.
It’s Not About Being Perfect
You don’t have to be the ‘perfect pregnant woman’ who never takes meds. You just have to be the one who made an informed choice. The goal isn’t zero risk-it’s the best possible outcome for you and your baby. That means treating your mental health like the medical condition it is. Not something to hide. Not something to feel guilty about. Something to manage, with support, with data, and with respect.What About Breastfeeding?
Most SSRIs pass into breast milk in tiny amounts. Sertraline and paroxetine are the lowest. Fluoxetine sticks around longer, so it’s less ideal if you’re nursing. Lithium requires careful monitoring in breastfeeding too. But here’s the good news: the benefits of breastfeeding often outweigh the tiny medication exposure. If you’re stable on meds and bonding with your baby, that’s a win. Talk to your provider about your feeding plan early-don’t wait until after birth.Are antidepressants safe during pregnancy?
Yes, many are. SSRIs like sertraline, citalopram, and escitalopram are considered first-line options because they have the most safety data. Paroxetine is the exception-it has a small increased risk of heart defects in the first trimester. The risks of untreated depression, including preterm birth and suicide, often outweigh medication risks.
Can I stop my meds if I’m pregnant?
Stopping without medical guidance is risky. About 80% of women with a history of depression relapse during pregnancy if they stop their meds. Many end up worse than before-some needing hospitalization. Always talk to your provider before making any changes.
What’s the safest medication for bipolar disorder during pregnancy?
Lamotrigine is the preferred choice. It has not been linked to major birth defects. Lithium can be used but needs close monitoring because pregnancy changes how your body processes it. Valproic acid should be avoided entirely-it increases the risk of neural tube defects by 10 to 20 times.
How do I know if I need medication or can manage with therapy?
It depends on your history. If you’ve had severe episodes, hospitalizations, or multiple relapses, medication is often necessary. Therapy alone isn’t enough for moderate to severe depression or bipolar disorder during pregnancy. A perinatal psychiatrist can help assess your individual risk and recommend the right mix of treatment.
Is it safe to breastfeed while taking mental health meds?
Yes, for most women. Sertraline and paroxetine pass into breast milk in very low amounts. Fluoxetine stays in the system longer, so it’s less ideal. Lithium requires monitoring. But the benefits of breastfeeding usually outweigh the minimal exposure. Talk to your doctor before birth to plan your feeding and medication schedule together.
Where can I find reliable information about medication risks?
The ACOG Mental Health Medication Decision Aid is the most trusted tool. It’s updated quarterly using data from the National Pregnancy Registry for Psychiatric Medications. Your provider should have access to it. Avoid relying on social media or anecdotal stories-they often misrepresent risk.
What if my doctor doesn’t mention shared decision-making?
Ask for it. Say: ‘I want to understand my options and risks so I can make the best choice for me and my baby.’ If your provider dismisses you, request a referral to a perinatal psychiatrist. These specialists are trained in this exact conversation-and 87% of obstetricians now consult them.

2 Comments
Just took my last Zoloft pill last week because my OB scared me into it. Now I’m crying in the shower at 3am. Worst decision ever.
I know how that feels. I stopped my Lexapro too, thought I could ‘be strong’-turned out I just became a ghost of myself. Talking to a perinatal psych saved me. You’re not alone.