
Lithium-NSAID Risk Calculator
NSAID Interaction Calculator
Calculate how much different NSAIDs increase lithium levels and assess your risk of kidney damage
Risk Assessment Results
When you’re on lithium for bipolar disorder, your body is already walking a tightrope. Too little, and your mood can spiral. Too much, and you risk serious, even life-threatening toxicity. Now add a common painkiller like ibuprofen or naproxen - something millions take without a second thought - and that tightrope becomes a cliff. The interaction between lithium and NSAIDs isn’t just a theoretical concern. It’s a well-documented, high-risk combination that can silently wreck your kidneys and poison your system - often before you even notice anything’s wrong.
How Lithium and NSAIDs Work Against Each Other
Lithium is a simple salt, but it’s one of the most effective mood stabilizers ever developed. It’s been used for over 50 years, and it still outperforms newer drugs when it comes to preventing suicide and stabilizing long-term bipolar cycles. But lithium doesn’t just float around in your blood. Your kidneys filter it out, day after day, keeping levels just right. That’s why regular blood tests are non-negotiable for anyone on lithium.
NSAIDs - like ibuprofen, naproxen, and indomethacin - work by blocking enzymes called COX-1 and COX-2. These enzymes help make prostaglandins, which keep your kidneys working smoothly. Prostaglandins keep blood flowing to your kidneys, helping them filter waste, including lithium. When NSAIDs shut down prostaglandin production, your kidneys slow down. And when they slow down, lithium doesn’t get cleared out like it should.
Studies show that just a few days of taking an NSAID can reduce lithium clearance by 25% to 60%. That means lithium builds up fast. In some cases, levels double within 48 hours. And you won’t feel it right away. No sudden pain. No obvious warning. Just a slow creep toward toxicity.
The Real Danger: Kidney Damage That Doesn’t Heal
It’s not just about lithium poisoning. The real threat is the double punch to your kidneys.
Lithium itself is mildly toxic to kidney cells. It interferes with how those cells manage water and salt, and over time, it can cause chronic changes - even if your levels are steady. NSAIDs make this worse. By cutting blood flow to the kidneys, they trigger ischemic injury. That’s tissue damage from lack of oxygen. Combine that with lithium’s direct cellular effects, and you’ve got a perfect storm.
A 2023 study in JAMA Network Open found that people taking both lithium and NSAIDs had more than three times the risk of acute kidney injury compared to those on lithium alone. The highest risk? The first 30 days after starting the NSAID. And for people over 65? The risk jumps even higher.
Worse still, this damage isn’t always reversible. One study of 17 patients hospitalized for lithium toxicity linked to NSAIDs found that 35% developed permanent kidney damage - meaning their kidney function dropped by 40% or more and never recovered. That’s not a side effect. That’s a life-altering outcome.
Not All NSAIDs Are Created Equal
You might think, “I’ll just pick a safer one.” But the truth is, most NSAIDs are dangerous with lithium - some more than others.
- Indomethacin is the worst offender - it can spike lithium levels by 40% to 60%.
- Piroxicam and naproxen aren’t far behind, with increases of 25% to 35%.
- Ibuprofen, the most commonly used NSAID, still raises lithium levels by 20% to 30% - enough to push someone into toxic range.
- Aspirin and celecoxib are the least risky, but even they can increase lithium by 10% to 15%, especially if you already have kidney issues.
There’s no safe NSAID for someone on lithium. Even if your doctor says “it’s fine,” the science says otherwise. And here’s the kicker: the interaction doesn’t vanish when you stop the NSAID. Prostaglandin suppression lasts 7 to 10 days. So if you took ibuprofen for a headache last week and now feel off - it could still be the NSAID.
What About Acetaminophen? Is It Safe?
Yes - and it’s your best bet.
Acetaminophen (Tylenol) doesn’t affect kidney blood flow or lithium clearance. Multiple studies show it causes less than a 5% change in lithium levels. That’s negligible. For chronic pain, acetaminophen is the first-line recommendation from the Canadian Network for Mood and Anxiety Treatments (CANMAT) and the European Psychiatric Association.
But even acetaminophen has limits. Don’t exceed 3,000 mg per day. Higher doses can damage your liver - especially if you drink alcohol or have existing liver disease. Still, compared to NSAIDs, it’s the clear winner.
For stronger pain, tramadol is sometimes used as a second option. It can slightly raise lithium levels (10% to 15%) mainly by causing dehydration, not kidney interference. But it’s not ideal long-term - it carries risks of dependence and seizures. Opioids? Only as a last resort, and only with close monitoring.
Who’s Most at Risk?
This isn’t a risk that affects everyone equally. Certain people are sitting on a ticking time bomb:
- People over 65: Kidney function naturally declines with age. Even a small drop in filtration can push lithium into toxic range.
- Those with existing kidney problems: If your eGFR is below 60 mL/min/1.73 m², your kidneys are already struggling. Adding an NSAID is like slamming the brakes on a car going downhill.
- People taking multiple medications: If you see a primary care doctor, a rheumatologist, and a psychiatrist - each might not know what the others prescribed. A 2023 study found that 32% of lithium patients who got NSAIDs were prescribed them by providers who didn’t know about their lithium use.
- Those who are dehydrated: Diuretics, heat, sweating, vomiting, or just not drinking enough water - all of these make lithium toxicity worse. NSAIDs make dehydration even more dangerous.
One study of 478 nephrology clinics found that over half of all lithium-related kidney injuries happened in patients over 65. And in Reddit communities, hundreds of users report tremors, confusion, and hospitalizations after taking ibuprofen - often because their doctor never warned them.
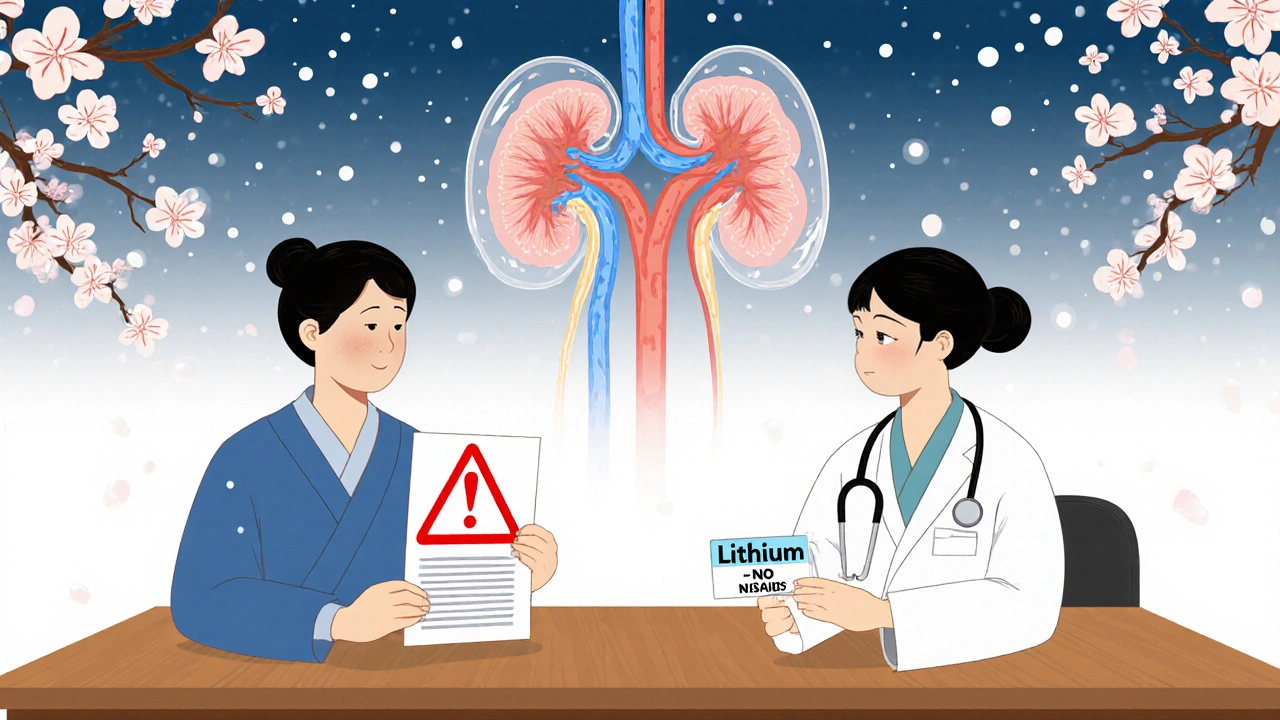
What Should You Do? A Clear Action Plan
If you’re on lithium, here’s what you need to do - right now:
- Stop taking NSAIDs unless your psychiatrist and nephrologist have approved it - and even then, only for 3 to 7 days max.
- Switch to acetaminophen for pain and fever. Stick to 3,000 mg/day or less.
- Ask your doctor for a kidney test - eGFR and serum creatinine - if you haven’t had one in the last 6 months.
- Get a lithium level check within 72 hours if you’ve taken an NSAID in the past two weeks.
- Carry a medication card that lists lithium and warns against NSAIDs. Show it to every new provider.
- Hydrate. Drink 2 to 3 liters of water daily, especially if you’re active or in hot weather.
And if you’re a provider? Document this. Warn your patients. Use your EHR to flag lithium users. Don’t assume someone else told them. Don’t assume they know. Too many people are getting hurt because this interaction is treated like a footnote - when it should be a red alert.
The Bigger Picture: Why This Keeps Happening
It’s not just patient ignorance. The system is failing.
Electronic health records have alerts for lithium-NSAID interactions - but 95% of U.S. hospitals have them, and yet co-prescribing hasn’t dropped enough. A 2019 FDA review found that alerts only reduced the practice by 35%. Why? Because they’re easy to bypass. A doctor clicks “override” because the patient is in pain. The system doesn’t force a conversation. It just lets the risk slide.
And patients? They don’t know. A 2023 survey found that only 58% of primary care doctors correctly identified NSAIDs as high-risk for lithium users. If the doctors don’t know, how can patients?
Meanwhile, lithium users are aging. Nearly two-thirds are now over 50. Most have arthritis, back pain, or headaches - conditions that drive NSAID use. The demand for pain relief is growing. The risk is growing. But the safeguards? They’re still patchy.
Some health systems are getting it right. Kaiser Permanente cut co-prescribing from 32% to under 12% by forcing education and hard alerts. The Veterans Health Administration? Not so much. Their numbers barely budged.
What’s Next? Hope on the Horizon
There’s some good news. Researchers are working on solutions.
A new drug in phase 2 trials - a prostaglandin E1 analog - is showing promise. Early results suggest it can keep kidney blood flow normal during NSAID use without interfering with lithium clearance. If it works, it could one day allow safer NSAID use for lithium patients.
But that’s years away. Right now, the only proven solution is avoidance.
Lithium remains the gold standard for preventing suicide in bipolar disorder. It reduces suicide risk by nearly half compared to alternatives. We can’t give it up. But we can protect the people who rely on it.
That means choosing acetaminophen over ibuprofen. It means asking for a kidney test before taking any new painkiller. It means speaking up when a doctor prescribes something that could harm you.
Because when it comes to lithium and NSAIDs, there’s no middle ground. There’s no “sometimes safe.” There’s only risk - and how much you’re willing to accept.

9 Comments
I was on lithium for three years and never knew NSAIDs could do this. My doctor just said "take Tylenol if you need pain relief" but never explained why. I took ibuprofen for a back flare-up last winter and ended up in the ER with tremors and confusion. They said my lithium level was 1.8. I didn’t even connect the dots until a nurse pulled up my med list and went pale. This post saved my life. Don’t wait until you’re in the hospital to learn this.
My mom’s on lithium and has osteoarthritis. She used to pop naproxen like candy. I printed out this article and left it on her fridge with a highlighter on the acetaminophen part. She rolled her eyes but hasn’t taken an NSAID since. She says her kidneys feel better. Small wins.
As someone from India where OTC painkillers are sold like candy, this is critical. I’ve seen friends take ibuprofen for headaches without knowing they’re on mood stabilizers. We need more awareness in places where doctors aren’t always accessible. Maybe translate this into local languages? This isn’t just a Western issue-it’s a global health blind spot.
I’m a nurse in a psych unit. We had a patient last month who got admitted after taking naproxen for two weeks. His lithium level was 2.1. He didn’t know it was dangerous. His PCP prescribed it. The system failed him. This post should be mandatory reading for every provider who writes prescriptions. We need better communication between specialties. It’s not just patients who need education-it’s the entire care network.
NSAIDs + lithium = avoid. Acetaminophen = safe. End of story.
While the clinical evidence presented here is unequivocal and aligns with current guidelines from CANMAT and the European Psychiatric Association, I would respectfully emphasize the importance of interdisciplinary collaboration. The failure of electronic health record alerts to meaningfully reduce co-prescribing rates suggests a systemic deficit in provider education and workflow integration. I urge institutions to implement mandatory CME modules on lithium pharmacokinetics and to embed hard-stop protocols for NSAID prescriptions in patients with documented lithium use. Patient safety cannot be left to optional clicks.
So let me get this straight. I can’t take Advil for my period cramps, but I can take Tylenol? Cool. So now I’m supposed to be grateful that my only pain relief option is a drug that can kill my liver if I accidentally take two extra pills? Thanks, medicine. At least the FDA didn’t warn me about that. I’m sure my kidneys are just fine. *sips water while holding a bottle of Tylenol* 🙃
Wait, wait, wait-so if I took ibuprofen last week for a headache, and now I’m feeling kinda off-like, fuzzy-headed and shaky-could it STILL be from that? Like, even though I stopped it?!! That’s wild. I didn’t know it stuck around for 7–10 days. My doc never told me that. I thought once you stop taking it, it’s gone. That’s... that’s a lot. I’m gonna go check my lithium levels tomorrow. I didn’t even realize I was at risk. I thought I was fine because I only took it once. Oh my god.
The epistemological rupture between pharmacological mechanism and clinical pragmatism is profoundly dissonant in this domain. Lithium’s narrow therapeutic index, mediated by renal tubular reabsorption dynamics, intersects catastrophically with NSAID-induced COX-2 inhibition, precipitating a cascade of hemodynamic dysregulation within the juxtaglomerular apparatus. The resulting oliguric state-concomitant with lithium’s intrinsic nephrotoxic potential-creates a synergistic insult that transcends additive pharmacokinetics; it is, in fact, a biodynamic catastrophe. The 35% incidence of irreversible renal impairment in the JAMA cohort is not merely statistical-it is an ontological betrayal of the patient’s physiological integrity. Until regulatory architectures enforce mandatory pharmacogenomic flagging and provider attestation, this remains a systemic failure of bioethical stewardship. Acetaminophen, while metabolically benign in this context, is not a panacea-it is merely the least inadequate option within a deeply compromised therapeutic landscape.