What Gestational Diabetes Really Means for Your Plate
When you’re pregnant and diagnosed with gestational diabetes, it’s not about cutting out carbs completely. It’s about choosing the right ones, at the right times, in the right amounts. About 1 in 12 pregnancies in the U.S. ends up with this diagnosis, according to the CDC. That’s more than 240,000 women every year. And the good news? Most of them can manage it without insulin-just by changing how and when they eat.
The goal isn’t to starve yourself or live on lettuce. It’s to keep your blood sugar steady so your baby grows safely. Too much sugar in your blood can lead to a big baby, which increases the chance of a C-section or birth injuries. It can also mean your newborn might have low blood sugar right after delivery. But when you get your numbers in range, those risks drop by more than 20%.
Your Blood Sugar Targets: What Numbers to Aim For
If you’ve been told to monitor your blood sugar, here’s what you’re really looking for:
- Fasting: Below 95 mg/dL (first thing in the morning before eating)
- 1 hour after eating: Below 140 mg/dL
- 2 hours after eating: Below 120 mg/dL
These aren’t arbitrary numbers. They come from the International Association of Diabetes and Pregnancy Study Groups (IADPSG), based on years of research showing these levels reduce complications. Most women who stick to a structured meal plan hit these targets without medication. One 2021 study found that 70% of women using meal planning alone stayed in range.
Don’t panic if you spike once. One high reading doesn’t mean you’re failing. It’s about patterns. Keep a log. Notice what meals make your numbers climb. That’s how you learn what works for your body.
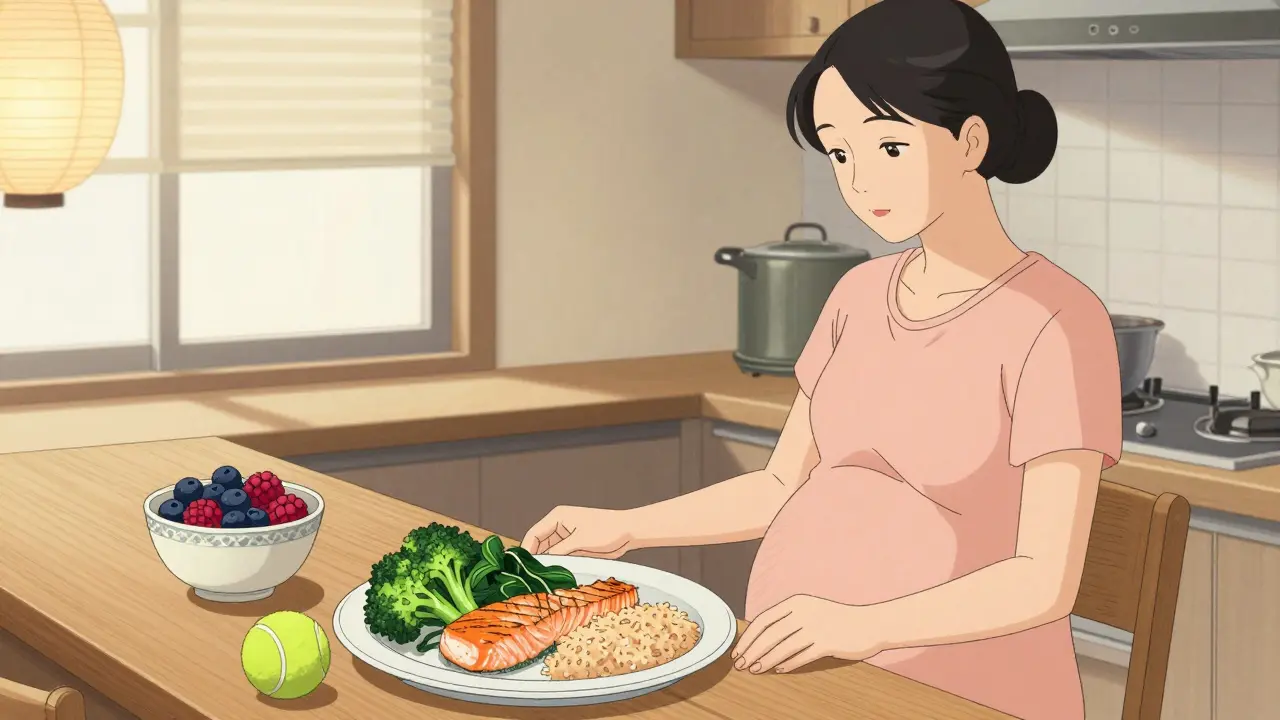
The Plate Method: Simple, Visual, and Effective
Trying to count grams of carbs while nauseous or tired? The plate method was made for you.
Take a standard 9-inch plate. Divide it like this:
- Half the plate: Non-starchy vegetables-broccoli, spinach, peppers, zucchini, cauliflower. These have fiber and almost no impact on blood sugar.
- One-quarter: Lean protein-chicken, fish, tofu, eggs, lean beef. Protein helps slow down carb absorption.
- One-quarter: Carbohydrates-whole grains, beans, fruit, or starchy veggies like sweet potato or corn.
This method was tested in a 2017 trial with over 1,200 women. It worked just as well as counting carbs-but 37% more women stuck with it because it didn’t require scales or apps. One woman on Reddit put it simply: “Measuring rice was impossible with morning sickness. I just fill half my plate with broccoli and it works.”
Portion sizes matter even with this method. One carb serving equals:
- 50g cooked brown rice (about two heaped tablespoons)
- 75g boiled potatoes
- One medium slice of whole grain bread
- One small apple or half a banana
Use a tennis ball as a visual guide for half a cup of cooked grains or beans. It’s easier than measuring cups when you’re juggling nausea and sleep deprivation.
Carbohydrate Counting: For When Precision Matters
If you had prediabetes before pregnancy, or your blood sugar spikes even with the plate method, you might need more precision. That’s where carbohydrate counting comes in.
Standard guidelines suggest:
- 45-60 grams of net carbs per meal
- 15 grams per snack
Net carbs = total carbs minus fiber. So if a serving of oats has 20g total carbs and 5g fiber, you count it as 15g net carbs. Fiber slows digestion and helps keep blood sugar steady. Aim for at least 6g of fiber per meal.
Women with pre-pregnancy insulin resistance (HbA1c over 5.7%) often do better with this method. But it’s harder. You need to read labels, weigh food, and track everything. Many find it overwhelming-especially with morning sickness. That’s why the plate method is recommended as a first step for most.

Meal Timing: Why Snacks Are Just as Important as Meals
Don’t skip snacks. In fact, many women with gestational diabetes need three meals and three snacks every day.
Why? Pregnancy hormones make your body more resistant to insulin, especially in the third trimester. Your liver starts pumping out more glucose overnight. If you go too long without eating, your blood sugar can rise even if you didn’t eat carbs.
Spread your carbs out. Eating 60g of carbs all at lunch will spike your sugar more than eating 20g at breakfast, 20g at lunch, and 20g at dinner. That’s why experts say timing matters more than total amount.
Try this snack combo: 1 ounce of cheese (about 2 slices) + 15g carbs (like half a whole grain English muffin or 1 small apple). This keeps blood sugar steady for hours. One mom in Kaiser Permanente’s program kept her fasting numbers at 87 mg/dL all through her third trimester using this exact approach.
What Foods to Choose (and Avoid)
Not all carbs are equal. Here’s what works:
- Best carbs: Oats, quinoa, brown rice, whole grain bread, beans, lentils, sweet potatoes, berries, apples, pears
- Good protein: Chicken, turkey, fish, eggs, tofu, Greek yogurt, cottage cheese
- Healthy fats: Avocado, olive oil, nuts, seeds
Avoid:
- Sugary drinks (even fruit juice)
- White bread, white rice, pastries
- Processed snacks labeled “diabetic-friendly” (they’re often high in sodium and artificial sweeteners)
- Large portions of dried fruit (raisins, dates)
One 2023 Lancet study warned that “diabetic-friendly” packaged foods have 27% more sodium than whole foods. They might be low in sugar, but they’re not healthy. Stick to real food.
Real-Life Meal Ideas That Actually Work
Here’s what a day might look like:
Breakfast
- 2 scrambled eggs
- 1 slice whole grain toast
- Half a small avocado
- 1 small orange
Carbs: ~45g | Fiber: 9g
Mid-Morning Snack
- 1 cup plain Greek yogurt
- 1/2 cup blueberries
- 1 tablespoon chia seeds
Carbs: ~15g | Fiber: 8g
Lunch
- 3 oz grilled chicken
- 1 cup roasted broccoli and Brussels sprouts
- 1/2 cup cooked quinoa
- 1 tablespoon olive oil and lemon dressing
Carbs: ~50g | Fiber: 10g
Afternoon Snack
- 1 small apple
- 1 tablespoon almond butter
Carbs: ~15g | Fiber: 4g
Dinner
- 4 oz baked salmon
- 1.5 cups sautéed spinach and mushrooms
- 1/2 cup black beans
- 1 small whole grain tortilla
Carbs: ~45g | Fiber: 12g
Evening Snack (if needed)
- 1 oz cheddar cheese
- 1 small pear
Carbs: ~15g | Fiber: 5g
This plan gives you about 190g net carbs total per day-well within the recommended range. And it’s full of fiber, protein, and healthy fats to keep you full and your sugar stable.
Cultural Foods? Yes, You Can Still Eat Them
Meal plans aren’t one-size-fits-all. A Filipino mom on Amazon reviewed a GDM cookbook saying: “The adobo chicken with half a cup of brown rice hit my carb target while feeling like home.” That’s the point.
Beans and rice? Yes. Lentils and whole wheat roti? Yes. Steamed fish with brown rice and stir-fried greens? Yes.
The key is portion control and pairing carbs with protein and fat. Don’t swap your culture’s food for bland “diabetic meals.” Adapt them. Use less rice. Add more veggies. Swap white rice for brown. Your body will thank you-and so will your taste buds.

What Doesn’t Work (And Why)
Some women try to go super low-carb to control blood sugar. That’s dangerous. Cutting carbs too much can mean not getting enough folate and iron-critical for your baby’s brain and spine development. One 2022 study found that women eating under 1,700 calories a day had an 18% higher risk of neural tube defects.
Others obsess over tracking every gram. That can trigger disordered eating. One 2021 study found 15% of women with gestational diabetes and a history of eating disorders saw their symptoms worsen when forced to count carbs.
And don’t rely on “sugar-free” products. Many contain sugar alcohols that can cause bloating and diarrhea. Some even raise blood sugar in the long run.
Tools That Help (And Ones That Don’t)
You don’t need fancy gadgets. But some things make life easier:
- Visual guides: Tennis ball = 1/2 cup cooked grains
- Food scale (for first week only, to learn portions)
- Free app like MyFitnessPal (to track net carbs, not calories)
- Online support: The r/GestationalDiabetes subreddit has over 147,000 members. 89% say it reduced their anxiety.
Avoid expensive meal delivery services marketed to GDM. They’re often overpriced and don’t teach you how to eat long-term. The goal is to build skills, not dependency.
When to Call Your Provider
Most women manage gestational diabetes with diet and movement alone. But if your numbers stay high after two weeks of following your plan, talk to your doctor. You might need insulin or metformin-and that’s okay. It doesn’t mean you failed. It means your body needs extra help.
Also call if you’re losing weight unintentionally, feeling dizzy, or getting frequent headaches. These could be signs of low blood sugar or dehydration.
What Happens After Baby Arrives
Good news: gestational diabetes usually goes away after birth. But your risk of type 2 diabetes later in life goes up-by 50% over the next 10 years. That’s why you’ll need a follow-up glucose test 6-12 weeks after delivery.
Keep eating the way you did during pregnancy. Stay active. Breastfeed if you can-it lowers your risk of type 2 diabetes. And remember: the habits you built for your baby? They’re the ones you’ll keep for yourself.

2 Comments
This is the most ridiculous piece of pseudoscience I've seen all year. Who the hell told you to eat half a banana with cheese? That's just sugar with extra steps. You're not feeding a baby, you're feeding a diabetic vending machine. And don't even get me started on 'net carbs'-that's a scam invented by keto bros to sell protein powder.
America needs to stop coddling pregnant women. If you can't handle eating a chicken breast and broccoli, maybe you shouldn't be having kids. I had three kids in the 80s and we didn't have any of this carb-counting nonsense. We ate rice, beans, and meat-no apps, no scales, no panic. Now we're turning pregnancy into a math test.