
What Is GERD, Really?
Gastroesophageal reflux disease, or GERD, isn’t just occasional heartburn. It’s when stomach acid keeps flowing back into your esophagus-often enough to cause irritation, pain, or even damage. If you’re dealing with symptoms more than twice a week, or if over-the-counter remedies aren’t helping, you’re likely dealing with GERD. About 1 in 5 people in the U.S. have it, and the numbers are rising as obesity rates climb. The good news? Most cases can be controlled without surgery-if you know what to do.
Start With Your Lifestyle-It’s the Foundation
Before you reach for a pill, fix what’s happening around your meals and your daily habits. These changes aren’t optional; they’re the first and most powerful step in managing GERD.
First, stop lying down right after eating. Waiting at least three hours after your last meal before going to bed cuts reflux episodes by half. Gravity helps keep acid where it belongs. If you’re still getting nighttime heartburn, raise the head of your bed by six inches using blocks or a wedge pillow. Don’t just pile on extra pillows-that just bends your neck and makes it worse.
Smoking weakens the muscle that blocks acid from rising. Just one cigarette can drop that muscle’s pressure by 30-40%. Quitting doesn’t just help your lungs-it helps your esophagus too. Same goes for alcohol. Two drinks a day is the max. More than that, and your lower esophageal sphincter (LES) starts to relax, letting acid slip through.
Weight matters. Losing just 10% of your body weight can improve symptoms by 40%. You don’t need to drop 50 pounds. Even a 10-15 pound loss can make a big difference. The pressure on your stomach drops, and acid stays put.
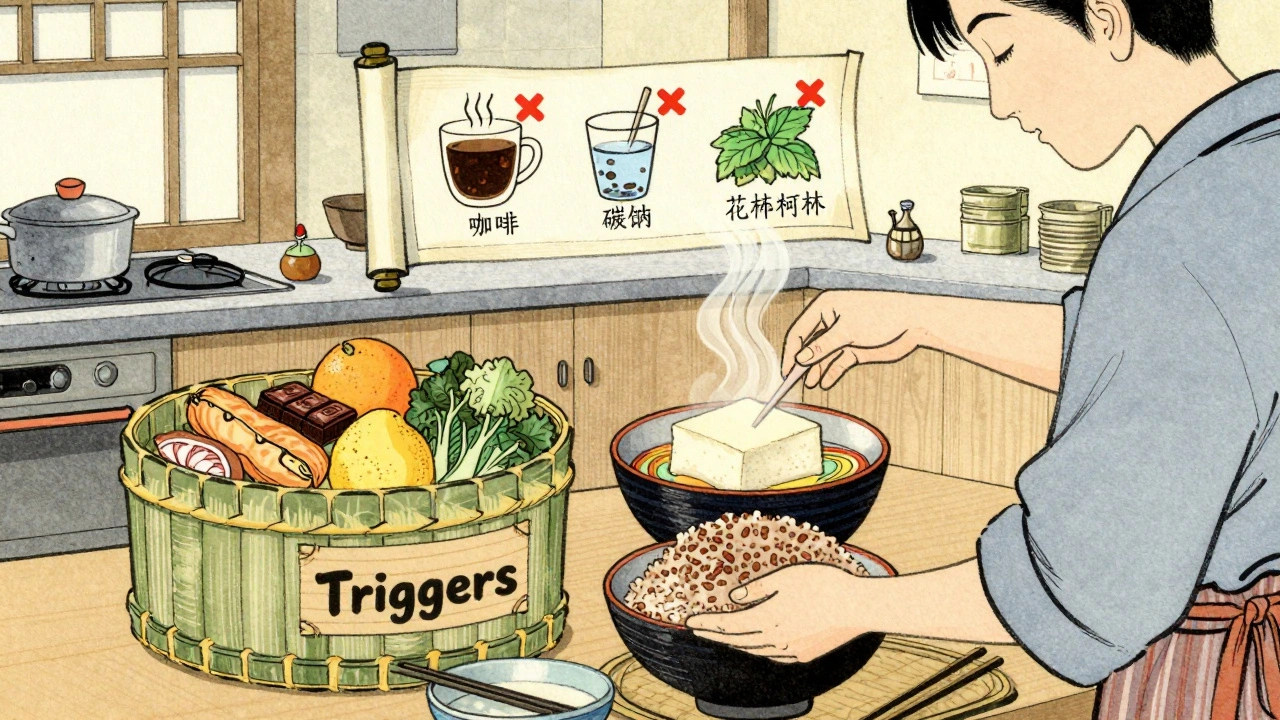
What You Eat (and Don’t Eat) Changes Everything
Not all trigger foods affect everyone the same way, but some are almost universal troublemakers.
- Fatty foods-anything fried, creamy sauces, bacon, or full-fat dairy-delay stomach emptying. That means food sits longer, acid builds up, and reflux happens. Aim for under 30% of your daily calories from fat.
- Caffeine-coffee, tea, energy drinks-boosts stomach acid by 23% within 30 minutes. Try switching to decaf or herbal teas like chamomile.
- Chocolate contains methylxanthine, which relaxes the LES. Even a small piece can trigger symptoms.
- Peppermint-yes, even mint tea-loosens the LES by 15-20%. It might soothe your stomach, but it’s not helping your reflux.
- Citrus fruits and juices (oranges, lemons, grapefruit) are highly acidic (pH 2-4). They don’t cause more acid-they irritate the lining already damaged by acid.
- Tomato products-sauces, soups, ketchup-are another common trigger. Even if you’ve eaten them for years, try cutting them out for two weeks.
- Carbonated drinks puff up your stomach, increasing pressure and forcing acid upward. Sparkling water isn’t safer than soda here.
- Spicy foods don’t produce more acid, but they make your esophagus more sensitive to it. That means even normal levels of acid feel painful.
Keep a food diary for two weeks. Write down everything you eat, when you ate it, and whether you had symptoms within two hours. You’ll likely find 2-3 specific triggers unique to you. Most people do.
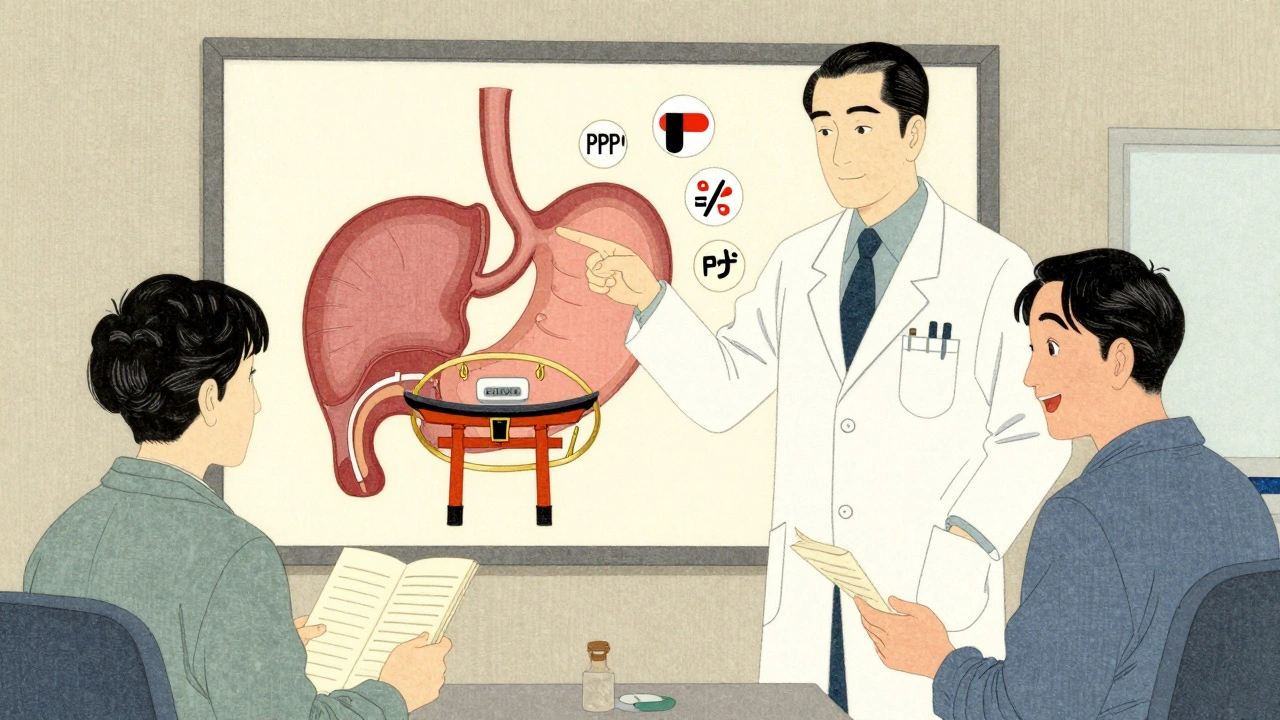
Medications: From Quick Fixes to Long-Term Solutions
If lifestyle changes aren’t enough, medications step in. There’s a clear order to how they’re used.
Antacids like Tums or Rolaids work fast-they neutralize acid in seconds. But they only last 30-60 minutes. Great for a quick fix after a meal, useless as a long-term plan.
H2 blockers like famotidine (Pepcid) cut acid production by 60-70%. They kick in within an hour and last 10-12 hours. Good for mild symptoms or occasional flare-ups. Many people use them before a big meal or at bedtime.
Proton pump inhibitors (PPIs) are the gold standard for moderate to severe GERD. Drugs like omeprazole, esomeprazole (Nexium), and pantoprazole reduce acid by 90-98%. They’re not fast-acting-you need 2-5 days of daily use to feel the full effect. Take them 30-60 minutes before your first meal of the day. If you take them after eating, they won’t work as well. That’s why 40% of people don’t get full relief-they’re taking them wrong.
PPIs work well, but long-term use (over a year) comes with risks. The FDA warns of higher chances of pneumonia, C. diff infection, kidney problems, and low magnesium levels. If you’ve been on a PPI for more than a year, ask your doctor about checking your magnesium and kidney function every six months.
Newer option: P-CABs. Vonoprazan (Voquezna), approved in late 2023, blocks acid more completely and faster than PPIs. It keeps stomach pH above 4 for 24 hours in 95% of users-compared to 65% with PPIs. It’s especially helpful for nighttime reflux, which affects 70% of PPI users. If your symptoms come back at night, this might be your next step.
Surgery: When Medications Aren’t Enough
For about 10-15% of people, medications just don’t cut it. Or they want out of the daily pill routine. That’s when surgery comes in.
The most common procedure is laparoscopic Nissen fundoplication. It wraps the top of your stomach around your esophagus to strengthen the LES. Success rates are 90-95% at five years. But 5-10% of people end up with trouble swallowing, and 15-20% get gas-bloat syndrome-feeling full, bloated, or unable to burp.
LINX is a newer option. It’s a small ring of magnetic titanium beads placed around the LES. It lets food pass down but snaps shut to block acid. Eighty-five percent of people stop needing daily PPIs after five years. It’s less invasive than fundoplication, but you can’t get an MRI after it’s implanted. Also, it’s not for people who’ve had prior stomach surgery.
TIF (Transoral Incisionless Fundoplication) is done through the mouth-no cuts. It’s good for people who want to avoid open surgery, but only about 127 doctors in the U.S. are trained to do it. Success rates are 70-75% at three years.
Not everyone needs surgery. But if you’ve tried everything else and still feel the burn, it’s worth discussing with a specialist.
What Experts Say About Personalized Care
Not all GERD is the same. Some people have erosive esophagitis-visible damage from acid. Others have non-erosive reflux disease (NERD), where the esophagus looks normal but still hurts. For NERD, acid might not be the main problem. Visceral hypersensitivity-your nerves being too sensitive-could be the real culprit.
That’s why one-size-fits-all doesn’t work. If PPIs aren’t helping, it doesn’t mean you’re “treatment-resistant.” It might mean you need a different approach: dietary changes, stress management, or even nerve-targeted therapies.
Doctors now recommend a step-by-step plan: start with lifestyle, add meds as needed, and consider surgery only after other options are exhausted. But some experts, like Dr. Lauren Gerson, argue that for patients with proven acid reflux, early surgery gives better long-term results than staying on pills forever.
Real People, Real Results
Reddit’s r/GERD community has over 140,000 members sharing what works. One user cut fat intake to under 20g a day and raised his bed-no meds, no symptoms. Another tried PPIs for five years, then got the LINX device. Two years later, he’s free from daily pills.
But it’s not always smooth. Some people report headaches, diarrhea, or vitamin B12 deficiency from long-term PPI use. LINX reviews show 78% are happy, but 22% still struggle with swallowing or bloating.
There’s no magic fix. But there is a clear path: track your triggers, fix your habits, use meds correctly, and know when to ask for help.
What’s Coming Next
The GERD market is growing fast, driven by rising obesity and aging populations. By 2028, it could hit $9.8 billion. Newer drugs like vonoprazan are gaining traction, and surgical options are becoming more precise.
The American College of Gastroenterology is updating its guidelines in late 2025 to reflect new science on non-acid reflux and personalized diets. That means your treatment plan could soon be even more tailored to your body.
For now, focus on what you can control: what you eat, when you eat, how you sleep, and whether you’re taking your meds right. Most people find relief with just these steps.
Can GERD be cured without medication?
Yes, for many people. Lifestyle changes-like losing weight, avoiding trigger foods, not eating before bed, and quitting smoking-can eliminate symptoms completely. Studies show up to 70% of patients achieve good control with diet and habits alone. But if you have visible esophageal damage or severe symptoms, medication is usually needed to heal the tissue.
How long should I take a PPI?
Take PPIs only as long as needed. For most people, 4-8 weeks is enough to heal the esophagus. If symptoms return, your doctor might recommend the lowest effective dose for maintenance. Long-term use (over a year) increases risks like kidney problems, infections, and low magnesium. Never stop suddenly-talk to your doctor about tapering off safely.
Is LINX surgery safe for everyone?
No. LINX isn’t for people who’ve had prior stomach surgery, those with a BMI over 40 (though recent updates allow up to 40 in Europe), or anyone who might need an MRI in the future. It’s also not recommended if you have severe esophageal motility disorders. A specialist must evaluate your anatomy and symptoms before recommending it.
Why do some people still get reflux on PPIs?
There are a few reasons. First, you might be taking it wrong-PPIs need to be taken 30-60 minutes before your first meal. Second, your reflux might not be caused by acid at all-non-acid reflux or bile reflux can mimic GERD. Third, you could have visceral hypersensitivity, where your nerves overreact to normal levels of acid. In these cases, PPIs won’t help, and you need a different diagnosis.
Can stress make GERD worse?
Yes. Stress doesn’t cause more acid, but it slows digestion, increases sensitivity to pain, and can lead to behaviors like overeating or late-night snacking-all of which trigger reflux. Techniques like diaphragmatic breathing, meditation, or yoga can reduce symptoms by up to 35% in mild cases. It’s not a cure, but it’s a powerful tool.
Are natural remedies like apple cider vinegar helpful?
No evidence supports apple cider vinegar for GERD. In fact, vinegar is acidic and can irritate an already inflamed esophagus. Some people swear by it, but that’s likely placebo or coincidence. Stick to proven methods: diet, timing, weight, and medication if needed.
Next Steps: What to Do Today
- Start a food and symptom diary for 14 days. Note meals, timing, and reflux episodes.
- Stop eating 3 hours before bed. Elevate your head if you get nighttime symptoms.
- Cut out the top 3 triggers: caffeine, fatty foods, and chocolate. See if symptoms improve.
- If you’re on a PPI, check if you’re taking it 30-60 minutes before breakfast. If not, adjust.
- Make an appointment with your doctor if symptoms persist after 4 weeks of lifestyle changes.
GERD isn’t something you just live with. With the right approach, you can take control-and live without the burn.

11 Comments
i just started cutting out coffee and chocolate and wow my night heartburn is way better. still eating fries tho lol 🤷♂️
This article is practically a manifesto. Anyone who still drinks soda before bed deserves their reflux. You're not 'sensitive'-you're just lazy.
If you're relying on PPIs, you've already lost. Real health comes from ancestral diets and fasting. This is why modern medicine is a scam.
so i raised my bed with books and now my head is at a 45 degree angle and my neck hurts but at least my chest doesnt burn??
I appreciate the thorough breakdown, but I'd like to add: for those of us with NERD, acid isn't the villain. My symptoms vanished after I started yoga and stopped eating dinner after 7 p.m.-no meds needed. It's not about willpower; it's about listening to your body.
There's a deeper layer here-GERD isn't just a physiological issue; it's a symptom of modern life's disconnection from rhythm. We eat while scrolling, we lie down while stressed, we numb with caffeine and alcohol. The body screams, and we call it 'heartburn.' Maybe the real cure is stillness.
I tried LINX. Two years in. I can eat pizza again. No PPIs. But I can't get an MRI. And sometimes I feel like I'm swallowing a tiny metal bracelet. Worth it? Yeah. Would I recommend it to everyone? Hell no. Talk to a surgeon who's done 200+ of these. Not the guy who just got certified last month.
I used to think apple cider vinegar was magic... until my esophagus felt like it was on fire for 3 hours. Now I just drink chamomile tea, sleep upright, and don't touch nachos after 6. Life's better. 🙌
You people are so naive. You think changing your diet will fix it? The real problem is your gut microbiome is destroyed from decades of processed food and antibiotics. No amount of wedge pillows will fix that. You need a fecal transplant. And a therapist. And to stop lying to yourself.
I've been managing GERD for 12 years. I used to take PPIs daily. Then I started keeping a food journal-turns out, my trigger wasn't spicy food or coffee. It was almonds. Yes, almonds. I ate them daily as a 'healthy snack.' Cut them out. Symptoms gone. Point is: your triggers are unique. Don't assume. Track. Test. Adjust. And don't let anyone tell you it's 'just in your head.' It's real, but it's also solvable.
The assertion that lifestyle modifications alone can cure GERD in 70% of cases is misleading. Such statistics often conflate symptom suppression with pathological resolution. Without endoscopic confirmation of mucosal healing, one cannot claim 'cure.' This is not pedantry-it is clinical rigour.