
Fluoroquinolone Tendon Risk Calculator
This tool helps you understand your personal risk factors for tendon rupture when taking fluoroquinolone antibiotics like ciprofloxacin or levofloxacin. Based on your answers, it will calculate your relative risk level.
Important: This is for informational purposes only and does not replace professional medical advice. Always discuss your medication risks with your doctor.
It’s not just a sore ankle. If you’ve been prescribed a fluoroquinolone antibiotic like ciprofloxacin or levofloxacin and feel a sharp pain in your heel, calf, or shoulder - especially if it came on suddenly - stop taking it and call your doctor. This isn’t muscle soreness from a workout. This could be the first sign of a tendon rupture, a serious and sometimes permanent injury linked directly to these widely used antibiotics.
Why Fluoroquinolones Are Different
Fluoroquinolones are powerful antibiotics. They’ve saved lives in cases of severe pneumonia, complicated urinary tract infections, and even anthrax exposure. But they’re not like penicillin or amoxicillin. These drugs don’t just kill bacteria - they interfere with how your body’s own cells function. That’s why they come with a black-box warning from the FDA, the strongest safety alert possible.Since 2008, regulators in the U.S., U.K., and Europe have tightened rules on fluoroquinolone use. The UK’s MHRA made it clear in 2019: don’t prescribe these drugs unless absolutely necessary. That means no more using them for simple sinus infections, ear infections, or mild bronchitis. If your doctor reaches for ciprofloxacin or levofloxacin for a routine infection, ask why. There are safer alternatives.
Which Tendons Are at Risk?
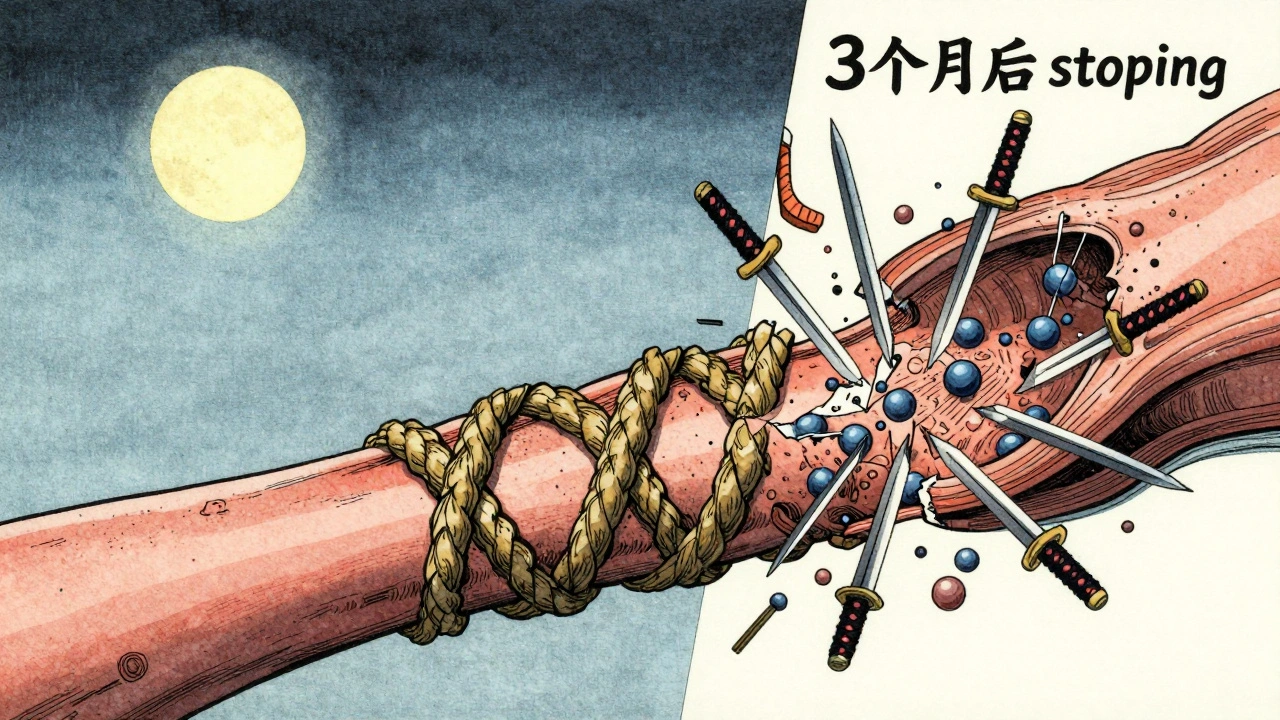
The Achilles tendon - the thick band connecting your calf to your heel - takes the biggest hit. Studies show it’s involved in nearly 90% of fluoroquinolone-related tendon injuries. But it’s not the only one. Shoulders, hands, thumbs, and even the rotator cuff can tear. What’s more, up to half of all cases affect both sides at once. You don’t need to be an athlete. A 72-year-old walking their dog or a 65-year-old gardening can rupture their Achilles tendon after just a few days on these drugs.When Does the Damage Happen?
Many people assume side effects show up after weeks. Not here. The median time from starting the antibiotic to first tendon pain is just six days. Eighty-five percent of cases occur within the first month. But here’s the scary part: symptoms can show up months after you’ve finished the course. One patient in a UK study reported pain three months after stopping levofloxacin. That’s why doctors now warn patients: if you feel tendon pain, even weeks after finishing the pills, get it checked.Who’s Most at Risk?
Not everyone gets tendon damage. But certain people are far more likely to. The biggest red flags:- Age 60+ - Your tendons naturally lose elasticity. Add fluoroquinolones, and rupture risk jumps dramatically. People over 80 have a 20-times higher risk than younger adults.
- Taking steroids - If you’re on prednisone for arthritis, asthma, or autoimmune disease, combining it with fluoroquinolones increases rupture risk by 46 times. This combination should never happen.
- Diabetes or kidney disease - These conditions already stress connective tissue. Fluoroquinolones make it worse.
- Previous tendon injury - If you’ve had a torn tendon before, you’re at higher risk for another - especially with these antibiotics.
Gender might also play a role. Some data suggests women report tendon pain more often than men, though we don’t yet know why. The same goes for race and genetics - researchers are still studying whether some people are born more vulnerable.

How It Happens - The Science Behind the Pain
Fluoroquinolones don’t just attack bacteria. They also interfere with mitochondria - the energy factories inside your cells. This leads to oxidative stress, which damages tendon tissue. They also block enzymes that help repair collagen, the main protein in tendons. And they bind to magnesium and calcium - minerals your body needs to keep tendons strong and flexible.Think of your tendon like a rope made of thousands of tiny fibers. Fluoroquinolones start fraying those fibers from the inside. You might not feel it until the rope snaps. That’s why pain often comes before rupture - and why ignoring early symptoms is so dangerous.
What the Numbers Say
A study of 6.4 million people in the UK found fluoroquinolone users were more than four times more likely to develop tendinitis and twice as likely to suffer a full rupture compared to non-users. Another study of 357,000 people in Taiwan showed a 42% higher rate of tendon disorders in those taking fluoroquinolones.But not all studies agree. A 2022 Japanese study found no significant link between third-generation fluoroquinolones and tendon rupture. Why the difference? Maybe genetics, diet, activity levels, or how data was collected. But when 120 million patient records across multiple countries show the same pattern, it’s hard to dismiss.
What to Do If You’re Prescribed One
If your doctor says you need a fluoroquinolone:- Ask: “Is this the only option? Are there safer antibiotics?”
- Tell them if you’re over 60, on steroids, have diabetes, or have had tendon problems before.
- Get the medication guide from the pharmacy - it lists all the risks.
- Don’t start running, lifting heavy things, or doing intense exercise while on the drug.
If you feel any pain, swelling, or stiffness in a tendon - even mild - stop the medication immediately. Don’t wait. Don’t assume it’s just soreness. Call your doctor. Get an ultrasound or MRI. Early action can prevent a full rupture.
What Happens After a Rupture?
A ruptured tendon isn’t just a bad day. It often means surgery, months of rehab, and sometimes permanent weakness or chronic pain. Some people never fully recover mobility. Recovery takes longer in older adults. And if you’ve had one rupture from fluoroquinolones, you’re at higher risk for another - even with different antibiotics later.Alternatives Exist
For most common infections, there are better choices:- Urinary tract infections: Nitrofurantoin, fosfomycin, or trimethoprim
- Sinus infections: Amoxicillin, doxycycline
- Respiratory infections: Azithromycin, amoxicillin-clavulanate
Fluoroquinolones should be reserved for life-threatening or multi-drug resistant infections - not for a stuffy nose or a urinary tract infection that could be treated with something simpler.
What Your Doctor Should Tell You
By law, doctors must warn patients about tendon rupture risk before prescribing fluoroquinolones. That means they should:- Explain the signs of tendinitis - pain, swelling, difficulty moving the joint
- Emphasize stopping the drug immediately if pain starts
- Advise avoiding strenuous activity during treatment
- Check for steroid use, age, and kidney function before writing the script
If they don’t mention any of this, ask. You have the right to know.
Final Thought: Don’t Assume It’s Safe Because It’s Common
About 25 million fluoroquinolone prescriptions are written in the U.S. every year. That’s a lot. But just because something is common doesn’t mean it’s safe. Millions of people take aspirin - but we don’t hand it out for every headache because we know the risks. Fluoroquinolones are the same. They’re powerful tools, but they’re not for every job.If you’re on one right now, pay attention to your body. If you’re about to start one, ask questions. Your tendons are your foundation - don’t risk them for a quick fix.
Can fluoroquinolones cause tendon rupture even after I stop taking them?
Yes. While most tendon issues start within the first month of use, symptoms can appear weeks or even months after you’ve finished the course. The UK’s MHRA and FDA both warn that tendon damage can occur after discontinuation. If you feel sudden pain in a tendon after stopping these antibiotics, don’t ignore it - get it checked.
Are all fluoroquinolones equally risky?
No. Levofloxacin and ciprofloxacin are the most commonly linked to tendon problems, making up about 88% of reported cases. Moxifloxacin carries less risk but is still not safe. None of them are risk-free. The FDA and MHRA treat the entire class as dangerous for tendons, regardless of which one you’re prescribed.
Is it safe to take fluoroquinolones if I’m under 60 and healthy?
Even if you’re young and healthy, fluoroquinolones still carry a real risk. The chance is lower than for older adults, but ruptures have happened in people in their 30s and 40s. The key is whether the infection truly requires this antibiotic. For most common infections, safer options exist. Don’t assume you’re immune just because you’re young.
What should I do if I feel tendon pain while on fluoroquinolones?
Stop taking the medication immediately. Do not wait to see if it gets better. Contact your doctor right away. Avoid putting weight on the affected area. Your doctor will likely order an ultrasound or MRI to check for damage. Continuing the drug increases the chance of a full rupture, which often requires surgery and long recovery.
Can I take painkillers like ibuprofen if I have tendon pain from fluoroquinolones?
No. While ibuprofen may reduce pain and swelling, it doesn’t stop the underlying damage. More importantly, masking the pain can lead you to keep using the affected tendon, increasing the risk of rupture. The priority isn’t pain relief - it’s stopping the drug and resting the tendon. Talk to your doctor about safe ways to manage discomfort while avoiding further injury.

15 Comments
Bro i took cipro for a UTI last year and my heel started killing me like 3 days in 😩 i thought it was just from walking too much then BAM one morning i couldn't push off my foot anymore. Doc said tendonitis turned to partial rupture. Never again. Just say no to antibiotics that feel like they were designed by a villain in a sci-fi movie 🤡
My mom got prescribed levofloxacin for a sinus infection and ended up in physical therapy for six months. She’s 68. They didn’t even warn her.
It’s wild how we’ve normalized prescribing powerful drugs like they’re candy. Fluoroquinolones are not just antibiotics they’re molecular wrecking balls that mess with your mitochondria your collagen repair systems and your mineral balance. And yet doctors still reach for them for a sniffle because it’s faster than explaining why amoxicillin is better. We need to stop treating patients like data points and start treating them like humans with tendons that don’t bounce back like rubber bands. This isn’t just about one drug it’s about a culture of convenience over care.
Just got off cipro last week and my Achilles has been a little tight. Going to skip the gym this week just in case 🙏
People who don’t read the black box warning deserve what they get. If you’re dumb enough to take cipro for a sinus infection you’re also dumb enough to ignore the pain. I’ve seen this movie before. Spoiler alert: the tendon doesn’t come back.
So we’re supposed to believe that a molecule designed to kill bacteria is also secretly a tendon assassin? How convenient. Next they’ll tell us oxygen causes cancer because lungs get inflamed. The real villain here is the medical-industrial complex selling fear to sell alternatives. Just say no to fearmongering.
It is a well-documented phenomenon that fluoroquinolones induce oxidative stress within tendinous tissues via mitochondrial dysfunction and chelation of divalent cations. The clinical correlation is robust across epidemiological datasets spanning multiple continents. To dismiss this as anecdotal is to misunderstand the nature of pharmacovigilance.
Wait so my dad died after a tendon rupture and he was on cipro?? I thought it was just old age. But he was on prednisone too?? Oh god I’m crying. I didn’t know. I feel so guilty. Can someone tell me if this is my fault? I should’ve stopped him??
Ah yes. The Western medical establishment’s greatest tragedy. We weaponize chemistry against microbes and then wonder why the human body collapses under the weight of its own arrogance. Fluoroquinolones are not drugs - they are the scream of a civilization that forgot how to heal. I weep for the tendons.
Actually the Japanese study disproved it. And the UK data is biased because they stopped prescribing these drugs so the people who got them were already high-risk. Also I’ve taken cipro 5 times and my tendons are fine. So your data is trash.
Let’s be clear: this isn’t a side effect. This is iatrogenic harm. The FDA’s black box warning has been on these drugs for 15 years. Hospitals still prescribe them for bronchitis. Doctors still ignore the risk factors. This is systemic negligence. And the fact that patients are still suffering is not an accident - it’s institutional malpractice.
Bro i got cipro for a UTI and my knee started popping. I thought it was nothing. Then i couldn’t squat. Got an MRI. Tendonitis. Doc said stop the med and rest. I did. 3 weeks later i’m back. Don’t be like me. Ask questions. Don’t be a hero.
My sister’s a nurse and she told me her hospital now has a checklist before prescribing fluoroquinolones - age steroids kidney function previous injury. If any of those are yes they go with something else. That’s progress. We need more of that. Not less.
Every time I hear about someone losing mobility from a preventable drug reaction I’m reminded that medicine is not just science - it’s a covenant between healer and human. Fluoroquinolones are not the enemy. Complacency is. If you’re a doctor reading this - pause before you write that script. If you’re a patient - speak up. Your body is not a lab rat.
My grandma tore her Achilles on cipro while watering her roses. She’s 82. No gym. No sports. Just a damn antibiotic. Now she walks with a cane and says ‘I didn’t know it could do that.’ I’m never letting anyone prescribe me one. Not even for plague.