
Fluoroquinolone-NSAID Risk Calculator
This tool estimates your risk of kidney damage and nerve injury when taking fluoroquinolone antibiotics with NSAIDs. Based on evidence from FDA, EMA, and clinical studies.
Your risk factors
What this means
Note: This calculator provides an estimate based on published research. Always consult your healthcare provider for personalized medical advice.
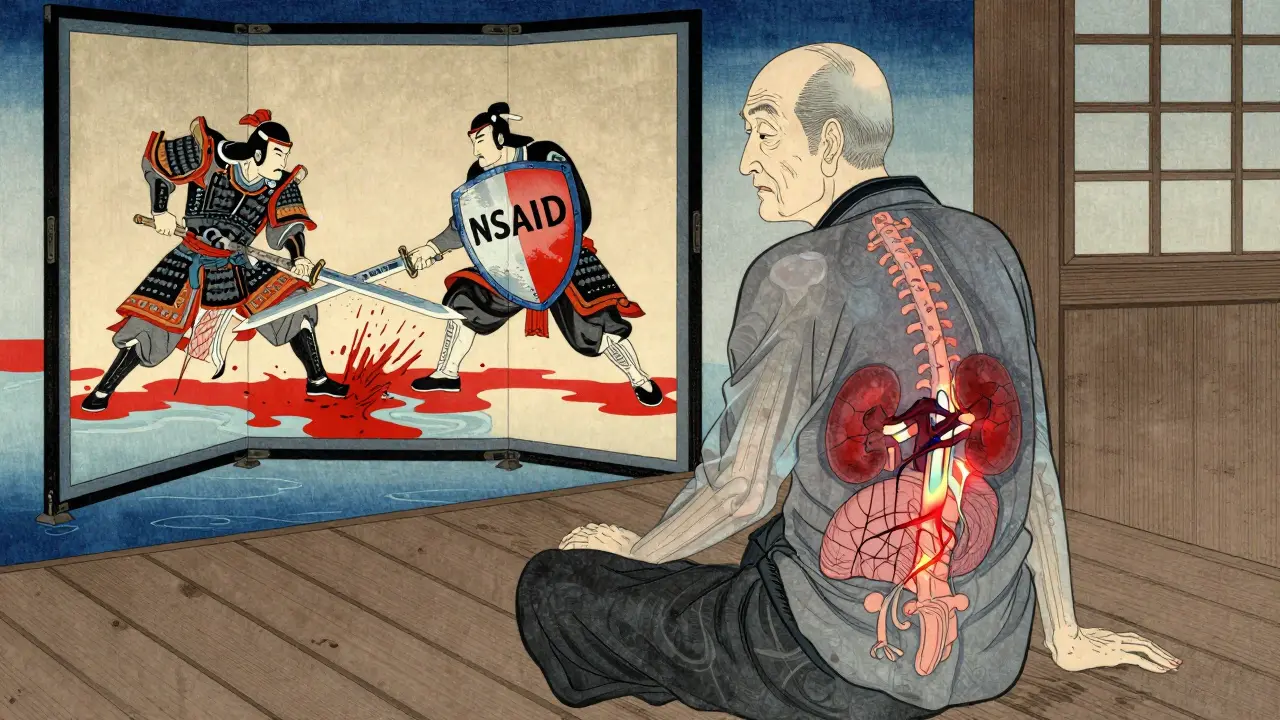
When you’re prescribed an antibiotic like ciprofloxacin or levofloxacin for a stubborn infection, and your doctor adds ibuprofen or naproxen for pain or fever, it seems like a simple, harmless combo. But what if this common pairing could quietly damage your nerves and kidneys-sometimes permanently? This isn’t speculation. It’s documented, regulated, and backed by real-world harm.
What Are Fluoroquinolone Antibiotics?
Fluoroquinolones include drugs like ciprofloxacin, levofloxacin, moxifloxacin, and ofloxacin. They’ve been used for decades to treat urinary tract infections, pneumonia, sinus infections, and other bacterial illnesses. They work well-fast, broad-spectrum, and often given as a short course. But behind their effectiveness is a growing list of serious, long-term side effects that regulators across the world have taken notice of.
Health Canada, the FDA, the European Medicines Agency, and the UK’s MHRA have all issued warnings since 2017. These aren’t vague cautionary notes. They’re clear: fluoroquinolones can cause disabling, sometimes irreversible damage to tendons, nerves, muscles, and the central nervous system. In the EU, over 21 years, 286 cases of severe, long-lasting reactions were officially recorded. That’s just the tip of the iceberg. Patient groups report far more.
How Fluoroquinolones Hurt Your Kidneys
Your kidneys filter your blood. Fluoroquinolones don’t just pass through them-they can actively damage them. Studies show a twofold increase in acute kidney injury requiring hospitalization in adults taking these antibiotics. The damage isn’t always obvious. It can show up as acute interstitial nephritis, where immune cells invade kidney tissue, or crystalluria, where the drug forms crystals in urine that block tiny tubules.
One 2013 study found that men on fluoroquinolones were twice as likely to be hospitalized for kidney failure compared to those not taking them. The risk isn’t just theoretical. A UK Yellow Card report details a 58-year-old man who took ciprofloxacin and ibuprofen together for a UTI. His creatinine level-normally around 82-spiked to 287 in days. He developed severe nerve pain too. Eighteen months later, he still hadn’t recovered.
How NSAIDs Hurt Your Kidneys Too
NSAIDs like ibuprofen, naproxen, and diclofenac don’t just reduce pain-they reduce blood flow to the kidneys. They block prostaglandins, chemicals that help keep kidney blood vessels open. In healthy people, this isn’t a big deal. But if you’re dehydrated, older, or already have reduced kidney function, it can push your kidneys into crisis.
When you combine NSAIDs with fluoroquinolones, the risk doesn’t just add up-it multiplies. One study in JAMA Internal Medicine found that in elderly patients, the combination raised the risk of acute kidney injury by up to 3.5 times. That’s not a small bump. That’s a cliff edge.
Neurological Risks: When Antibiotics Mess With Your Brain
Fluoroquinolones can cross the blood-brain barrier. Once inside, they interfere with GABA receptors-the brain’s natural calming system-and overstimulate NMDA receptors, which excite nerve cells. This imbalance can trigger seizures, confusion, hallucinations, psychosis, and even delirium.
Ciprofloxacin is linked to confusion and mental fog. Levofloxacin has been tied to seizures, especially in people with kidney problems. Ofloxacin, while still risky, seems to cause fewer neurological issues-likely because it doesn’t penetrate the brain as deeply.
NSAIDs aren’t innocent here either. Headaches and dizziness are common. Rarely, they cause aseptic meningitis-brain inflammation without infection. Ibuprofen and naproxen are the most frequent culprits.
When both drugs are taken together, especially in someone over 60 or with an eGFR below 60, the brain gets hit from both sides. Fluoroquinolone levels rise because kidneys can’t clear them. NSAIDs worsen that by reducing kidney function. The result? Higher drug concentrations in the blood, more brain exposure, and a higher chance of serious neurological events.
Who’s at Highest Risk?
Not everyone will have a bad reaction. But certain people are far more vulnerable:
- People over 60-kidney function drops about 1% per year after 40
- Those with chronic kidney disease (eGFR below 60 mL/min/1.73m²)
- Patients with epilepsy, Parkinson’s, or a history of mental health disorders
- Anyone taking other nephrotoxic drugs like diuretics or ACE inhibitors
- People who are dehydrated or have low blood pressure
These aren’t edge cases. They’re common. A 65-year-old with mild kidney decline and arthritis is exactly the kind of patient who gets this combo prescribed.
Real Patients, Real Damage
Behind the statistics are people who didn’t get better-they got worse.
The Fluoroquinolone Effects Research Foundation surveyed 1,245 patients. 78% had symptoms lasting over six months. 32% said they were permanently disabled. Common complaints: burning nerve pain, muscle weakness, brain fog, insomnia, and chronic fatigue.
Reddit’s r/FQAntibioticDamage has over 14,500 members sharing stories of lives turned upside down after a routine course of ciprofloxacin. One woman described losing the ability to walk without a cane. Another couldn’t remember her children’s names for months. These aren’t anecdotes from fringe forums-they mirror official adverse event reports.

What Should You Do?
If you’re prescribed a fluoroquinolone and your doctor also recommends an NSAID, ask:
- Is there a safer antibiotic option? Nitrofurantoin for UTIs, amoxicillin-clavulanate for respiratory infections, or doxycycline for certain infections are often just as effective with far fewer risks.
- Can I use acetaminophen instead of ibuprofen? Acetaminophen doesn’t affect kidney blood flow or GABA receptors. It’s the safer painkiller when fluoroquinolones are needed.
- Have you checked my kidney function recently? A simple eGFR blood test takes seconds and can change everything.
- Are you aware of the 2019 MHRA and EMA restrictions? These drugs are now meant for infections with no alternatives.
Don’t assume your doctor knows all the risks. Many still prescribe fluoroquinolones as first-line because they’re cheap, effective, and familiar. But guidelines have changed. The UK’s MHRA says fluoroquinolones should only be used when other antibiotics won’t work. That’s not a suggestion-it’s a rule.
The Bigger Picture: Why This Is Still Happening
Despite FDA warnings since 2016, and EMA restrictions since 2019, fluoroquinolones are still prescribed over 22 million times a year in the U.S. That’s down from 28 million in 2015-but still too high. In India and China, they account for nearly half of global use.
Why? Because they’re cheap, easy to prescribe, and patients often demand quick fixes. But the cost isn’t just financial. A 2020 study estimated fluoroquinolone-related adverse events cost the U.S. healthcare system $1.8 billion annually. Nearly 40% of that came from kidney injuries. Nearly 30% from neurological damage.
The FDA is now reviewing label updates to include warnings about mitochondrial toxicity-a deeper mechanism that may explain why damage persists long after stopping the drug. This isn’t going away. It’s getting worse.
Alternatives That Work
For urinary tract infections: Nitrofurantoin or fosfomycin. Both are effective and don’t carry the same neurologic or renal risks.
For sinus or respiratory infections: Amoxicillin-clavulanate, doxycycline, or azithromycin. These are safer and just as effective for most cases.
For pain and inflammation: Acetaminophen (paracetamol) is the go-to. It doesn’t harm kidneys or interact with fluoroquinolones. For chronic pain, physical therapy or low-dose gabapentin may be better long-term options.
Don’t settle for ‘it’s just a pill.’ If the risk is permanent nerve damage or kidney failure, there’s no such thing as ‘just.’
Can fluoroquinolones and NSAIDs cause permanent damage?
Yes. Both fluoroquinolones and NSAIDs can cause lasting harm when used together. Fluoroquinolones are linked to permanent nerve damage (peripheral neuropathy), tendon rupture, and chronic kidney injury. NSAIDs can worsen kidney function long-term, especially in older adults. When combined, the risk of irreversible damage increases significantly. Many patients report symptoms lasting years or for life.
Is it safe to take ibuprofen with ciprofloxacin?
No, it’s not considered safe. Combining ibuprofen with ciprofloxacin increases the risk of acute kidney injury and neurological side effects like seizures and confusion. The combination is especially dangerous for people over 60, those with kidney problems, or anyone dehydrated. Acetaminophen is a safer pain relief option if you’re on ciprofloxacin.
What are the signs of kidney damage from these drugs?
Signs include reduced urine output, swelling in legs or ankles, fatigue, nausea, confusion, and unexplained itching. A simple blood test showing rising creatinine levels confirms kidney injury. If you’re taking these drugs and notice any of these symptoms, stop the NSAID immediately and contact your doctor.
How long do neurologic side effects last after stopping fluoroquinolones?
For some, symptoms resolve within weeks. But for others, they persist for months or years. Studies show 78% of patients report symptoms lasting more than six months. In 32% of cases, damage is permanent. Symptoms include tingling, burning pain, muscle weakness, brain fog, insomnia, and anxiety. Recovery is unpredictable and often incomplete.
Are there safer antibiotics than fluoroquinolones?
Yes. For urinary infections, nitrofurantoin or fosfomycin are preferred. For respiratory infections, amoxicillin-clavulanate, doxycycline, or azithromycin are effective and safer. Fluoroquinolones should only be used when other options have failed or aren’t suitable-this is now official guidance from the UK’s MHRA and the EMA.

4 Comments
Wow, this is eye-opening. I’ve been taking ibuprofen with cipro for my UTIs for years without thinking twice. Guess I got lucky so far. Thanks for laying it all out like this - really makes you pause before clicking ‘add to cart’ on that OTC painkiller.
Look i know this sounds like some alt med blog but i’ve seen this first hand. My uncle took cipro and naproxen after a bad knee infection and ended up in a wheelchair for 18 months. Nerve damage. Kidneys fried. Docs said it was ‘uncommon’ but then he found 5 other guys in the same hospital ward with the same story. The system is broken. Pharma pushes these drugs like candy and docs don’t even read the fucking footnotes anymore. I’m not mad at you for posting this - i’m mad at everyone who lets this keep happening.
Oh please. Another fearmongering post. If you’re taking fluoroquinolones and NSAIDs together, you’re probably already on 12 other meds and drinking 3 liters of Diet Coke. This isn’t a public health crisis - it’s a case of people not reading the damn leaflet. If your kidneys can’t handle two common drugs, maybe stop pretending you’re 25.
Thank you for this. I’m a nurse and I’ve seen too many elderly patients get this combo and never recover. I always ask about NSAIDs before prescribing fluoroquinolones - but half the time, the doctor just says ‘it’s fine.’ We need better education. Also - acetaminophen is your friend. 🙏