Most people assume that if a drug makes it through clinical trials and gets approved by regulators, it’s safe. But the truth is, some of the most serious risks only show up after thousands or even millions of people start taking it. That’s where drug safety signals come in - the early warning signs that something might be wrong, hidden in mountains of data no one saw during the trial phase.
What Exactly Is a Drug Safety Signal?
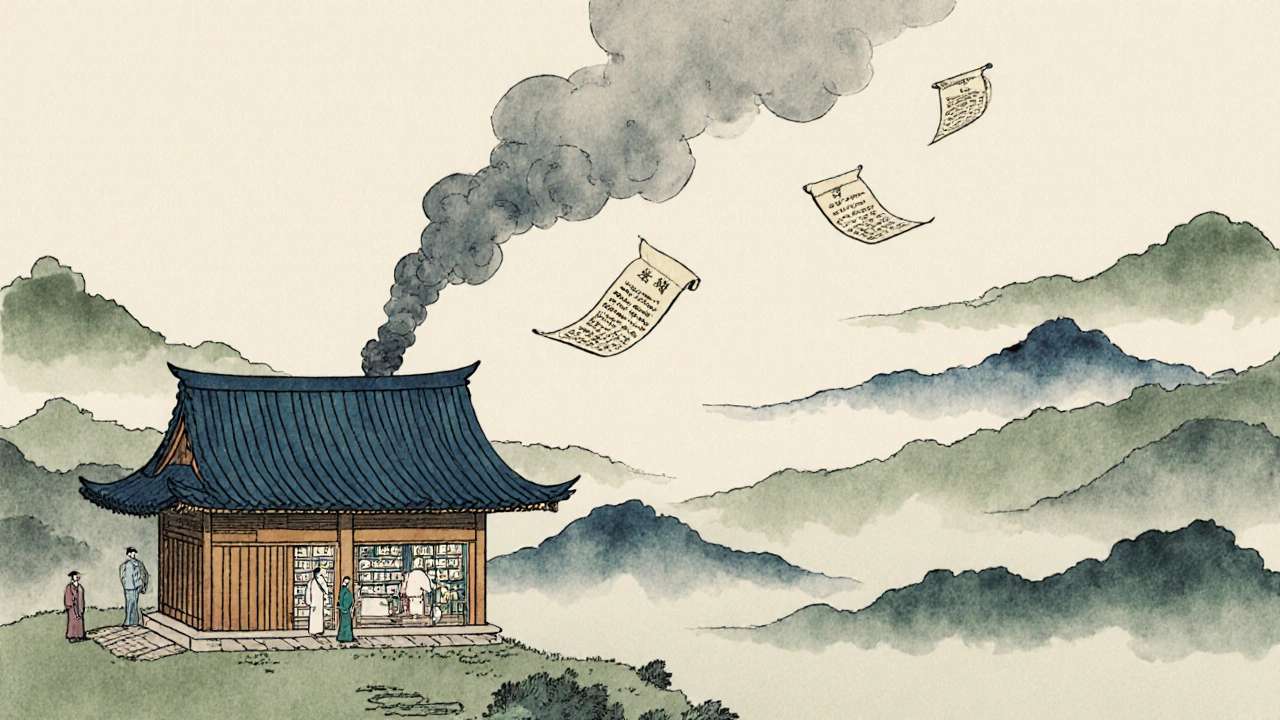
A drug safety signal isn’t a confirmed danger. It’s a red flag - a pattern in the data that says, ‘Hey, this might not be a coincidence.’ According to the Council for International Organizations of Medical Sciences (CIOMS), it’s information suggesting a new or previously unknown link between a medicine and an adverse event that’s strong enough to warrant investigation. Think of it like smoke coming from a building. You don’t know yet if there’s a fire, but you don’t ignore it. That’s what regulators and drug companies do when they spot a signal. It could be a spike in reports of liver damage after a new diabetes drug hits the market. Or a cluster of heart rhythm issues in elderly patients using a blood thinner. These aren’t random. They’re patterns. Signals come from two main places: spontaneous reports and clinical trial data. About 90% of the data feeding into systems like the FDA’s FAERS or the EMA’s EudraVigilance comes from doctors, pharmacists, or even patients reporting side effects after the drug is out in the real world. The other 10% comes from clinical trials - but here’s the catch: those trials rarely catch everything.Why Clinical Trials Miss the Big Risks
Clinical trials are tightly controlled. They involve a few thousand people at most, often healthy volunteers or patients with one specific condition. They’re short - usually a few months to two years. And they exclude a lot of people: those with other illnesses, older adults on multiple meds, pregnant women, kids. That means rare side effects? They vanish in the noise. If a drug causes a severe reaction in one in 10,000 people, you’d need to give it to 10,000 people to see it once. Most trials don’t reach that number. And even if they do, the event might not show up until years later. Take bisphosphonates - drugs for osteoporosis. The risk of jawbone death (osteonecrosis) wasn’t noticed until seven years after approval. Why? Because it only happens after long-term use, and it’s rare. By then, hundreds of thousands of people had already taken it. Or consider rosiglitazone, a diabetes drug. Early trials showed it lowered blood sugar. But after millions of prescriptions, data from spontaneous reports and studies began pointing to a higher risk of heart attacks. That signal emerged years after approval - not in the trials.How Signals Are Found in the Noise
Regulators don’t just read reports. They use math. Tools like reporting odds ratios (ROR), proportional reporting ratios (PRR), and Bayesian methods scan millions of entries to find unusual clusters. For example, if 100 people report a rare stroke after taking Drug X, but only 5 people report it after taking Drug Y - and Drug X has been taken 10 times more often - that’s a signal. But here’s the problem: most of these signals are false alarms. Studies estimate 60% to 80% of statistical signals turn out to be noise - caused by reporting bias, coincidences, or incomplete data. A 2019 signal linking canagliflozin to leg amputations looked terrifying at first. The numbers jumped. But later, a large trial (CREDENCE) showed the actual risk was only 0.5% higher than placebo. The signal was real - but the danger wasn’t. That’s why no regulator acts on a single signal. They look for triangulation: the same pattern appearing in spontaneous reports, published studies, electronic health records, and patient registries. The more sources that confirm it, the more serious the concern.
What Makes a Signal Turn Into a Warning?
Not every signal becomes a black box warning on a drug label. Four things make a difference:- Replication across sources - If three different databases show the same pattern, the chance it’s real jumps dramatically. Studies show this increases the likelihood of a label update by over four times.
- How serious the event is - Death, hospitalization, or permanent disability? Those get attention fast. Non-serious side effects like mild headaches rarely trigger action.
- Does it make biological sense? - If a drug affects the immune system and patients start getting rare autoimmune disorders, that’s plausible. If it’s a stretch? Regulators dig deeper.
- How new is the drug? - Drugs under five years old are 2.3 times more likely to get a safety update than older ones. That’s because we haven’t seen the long-term picture yet.
The Real-World Challenges
Finding signals sounds technical, but the human side is messy. Pharmacovigilance teams spend most of their time chasing false leads. A 2021 survey of 327 safety professionals found that 73% were frustrated by the lack of standard ways to judge whether a side effect is truly caused by the drug. Was it the drug? The patient’s other meds? An infection? A genetic quirk? Data quality is another nightmare. Many spontaneous reports are incomplete. A doctor might write ‘headache’ without noting if it was severe, how long it lasted, or if the patient stopped the drug and it went away (a key clue called dechallenge). Only 43% of reports include enough detail to assess causality properly. And then there’s the sheer volume. EudraVigilance handles over 2.5 million reports a year. FAERS has over 30 million. Sorting through that manually is impossible. That’s why AI tools are exploding. The EMA’s AI system now cuts signal detection time from two weeks to under two days. The FDA’s Sentinel Initiative pulls data from 300 million patient records - real-time, from hospitals and pharmacies. But AI isn’t magic. It still needs human judgment. A machine can spot a spike in kidney failure reports after a new antibiotic. But only a clinician can say whether it’s the drug, or if those patients were already critically ill.
What’s Changing Now - And What’s Next
The biggest shift? Integration. The future isn’t just spontaneous reports or clinical trials. It’s combining all data: electronic health records, pharmacy logs, wearable sensors, even patient-reported symptoms from apps. By 2027, over 65% of top-priority signals are expected to come from these integrated systems - up from just 28% in 2022. New drugs are also getting harder to monitor. Biologics, gene therapies, cell therapies - these aren’t pills. They’re complex living molecules. Their side effects are unpredictable. A drug that modifies immune cells might trigger inflammation months later. Or cause a rare autoimmune reaction. Traditional signal detection wasn’t built for that. And then there’s aging populations. Since 2000, prescription use in people over 65 has doubled. Many take five, six, or more drugs. Drug interactions? They’re invisible in trials. But in the real world, they’re the hidden cause of many adverse events. Regulators are adapting. The EU now requires every new drug application to include a detailed signal detection plan - not just a footnote. The FDA is pushing for standardized lab data reporting to better detect liver injuries. And the WHO’s global network now collects 350,000 reports a month from 155 countries.What This Means for Patients and Doctors
You don’t need to be a scientist to understand this: approval doesn’t mean perfection. It means the benefits outweigh the known risks - for the population studied. But real-world use is different. If you’re on a new drug, pay attention. Note any new symptoms. Talk to your doctor. Don’t assume it’s ‘just aging’ or ‘stress.’ Doctors, too - keep reporting. Even if it seems minor. A single report might not mean much. But 100? That’s a signal. Your notes matter. And if you’re a patient who’s had a bad reaction? You’re part of the system. Your story could save someone else’s life. The system isn’t perfect. It’s slow. It’s noisy. But it’s the best we have. And it’s getting smarter - one signal at a time.What’s the difference between a drug side effect and a safety signal?
A side effect is any unwanted reaction to a drug - even common ones like nausea or dizziness listed in the patient leaflet. A safety signal is a pattern of unexpected or rare side effects that appears in post-market data and suggests a possible new risk. Not all side effects become signals - only those that are unusual, serious, or appear more often than expected.
Can a drug be pulled from the market because of a safety signal?
Yes, but it’s rare. Most signals lead to label updates, restricted use, or new warnings - not removal. A drug is only withdrawn if the risk clearly outweighs the benefit and no safer alternatives exist. Examples include rofecoxib (Vioxx) for heart attack risk and cerivastatin (Baycol) for muscle damage. These decisions come after multiple signals are confirmed across several data sources.
Why do some signals take years to be confirmed?
Some risks only show up after long-term use, in older patients, or when combined with other drugs - all things clinical trials don’t capture. Also, rare events need time to accumulate enough reports to stand out from background noise. A signal for liver damage in elderly patients on multiple medications might take five years to reach statistical significance across global databases.
Are newer drugs more dangerous than older ones?
Not necessarily - but they’re less understood. Newer drugs (under five years) are more likely to get safety updates because we haven’t seen their full long-term profile. Older drugs have been used by millions, so their risks are better mapped. But that doesn’t mean older drugs are safer - just that we know more about them.
How can patients help with drug safety monitoring?
Report any new or unusual symptoms to your doctor - and ask them to report it to national pharmacovigilance systems. If you’re in the UK, you can report directly to the MHRA via the Yellow Card scheme. Even if you’re unsure if the drug caused it, your report adds data. Thousands of reports are needed to spot a signal.

12 Comments
Man, this is why I never trust new drugs. I saw a guy on Reddit take that new migraine med and end up in the ER with liver failure. Docs said it was 'rare' but rare doesn't mean it won't be YOU. They test on 20-year-old college kids and then sell it to grandmas on Medicare. That's not science, that's gambling.
Of course they miss the risks 😏 Big Pharma funds the trials, regulators get cozy with CEOs, and the FDA’s budget is cut every year. AI? More like AI-Driven Cover-Up™. They know. They just don’t care until lawsuits pile up. Remember Vioxx? 60k dead. And they still sell similar crap today. #PharmaControl
One must contemplate the epistemological boundaries of medical knowledge. The clinical trial, as a construct, is a reductionist artifact-a statistical mirage in the cathedral of human physiology. To presume safety on the basis of controlled, finite exposure is to mistake the map for the territory. The body, in its wild, polypharmaceutical reality, sings a symphony the lab can never hear. The signal, then, is not noise-it is the voice of complexity, demanding humility.
Keep reporting your side effects. Seriously. One person’s 'mild headache' is another person’s warning sign. Your voice matters. The system only works if we all participate. You’re not just a patient-you’re part of the safety net.
I’ve been on 7 different meds in the last 5 years. Two of them made me feel like my bones were melting. Docs shrugged. 'It's rare.' But rare doesn’t mean it didn’t happen to me. And now I’m paranoid every time I get a new script. We need better tracking. Not just AI. Real humans listening. Real doctors who don’t rush through appointments.
Let’s be real-this whole system is a glorified dumpster fire wrapped in a white coat. They use math to find needles in haystacks made of lies. And when they finally spot something? They slap on a tiny warning label and keep selling. Meanwhile, the guy who lost his kidney to that 'safe' NSAID? Yeah, he’s just another footnote in the annual report. Congrats, pharma. You’re still rich.
AI detecting signals in 2 days? LOL. They’ve had this tech for 10 years. Why are we only hearing about it now? Because they’re waiting for the next billion-dollar drug to blow up. Then they’ll play the hero and 'fix' the system. Classic. They don’t want safety-they want liability shields.
This is why America needs to stop outsourcing drug safety to bureaucrats who don’t even understand pharmacology. We have the best scientists in the world-why are we letting EU and WHO dictate our standards? If a drug passes FDA review, it should be safe. End of story. Stop the fearmongering. People need meds. Not more red tape.
So... we’re supposed to trust a system that missed osteonecrosis for 7 years? 😅 And now we’re gonna trust AI? I’ll stick with my grandma’s herbal tea. At least it didn’t come with a 47-page warning leaflet.
Hey, if you're on a new med, don't panic-but do track your symptoms. Write them down. Talk to your pharmacist. They’re the real MVPs. And if something feels off, push back. You’re not being difficult-you’re being smart. Your body knows before the data does. Trust it. And report. Even if it’s 'just' fatigue. It matters.
The integration of EHRs, pharmacy records, and wearable data represents a paradigm shift in pharmacovigilance. However, the lack of interoperability standards across healthcare systems remains a critical impediment. Without harmonized data schemas, even the most advanced algorithms will continue to operate in silos. The technical feasibility exists-what is lacking is institutional will.
They say 'approval doesn't mean perfection.' But isn't that the whole point? If they knew it wasn't perfect, why approve it? The entire system is a lie we tell ourselves so we can sleep at night. We don't want to admit that medicine is still guesswork with profit margins. We want miracles. But miracles aren't science. They're marketing.