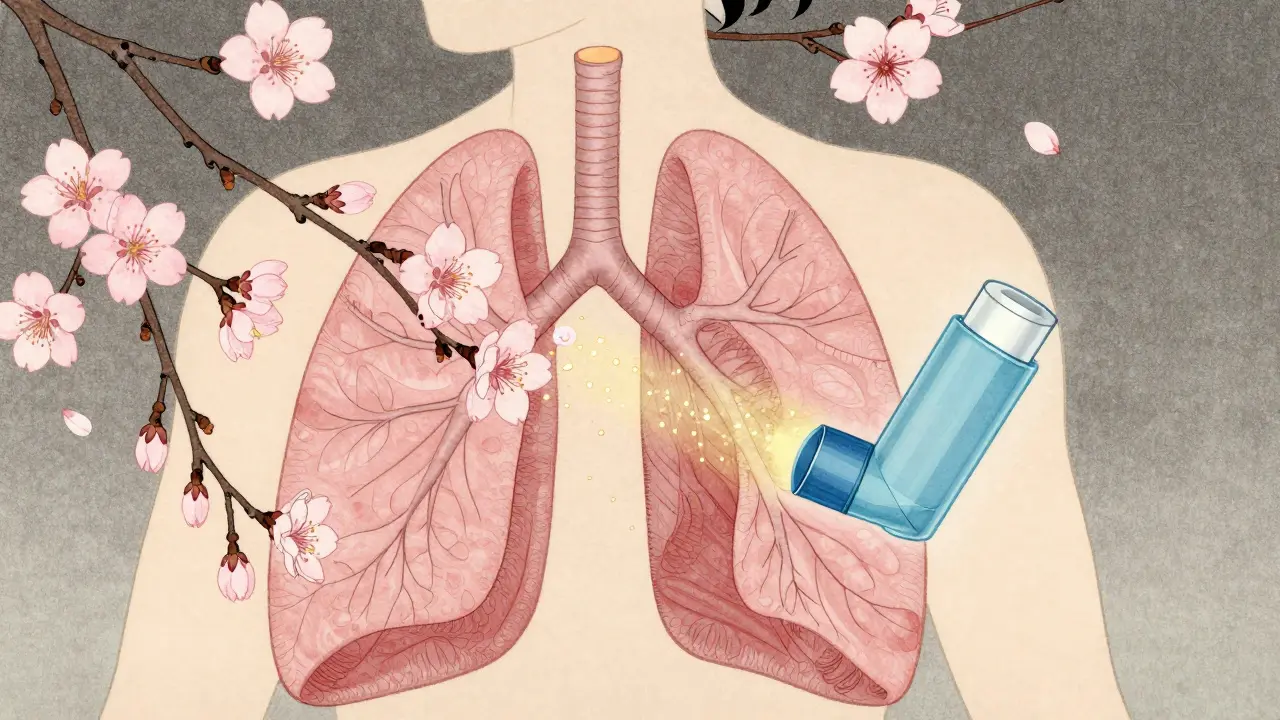
When your airways tighten up and breathing feels like trying to suck air through a straw, two types of medicines are doing the heavy lifting: bronchodilators and corticosteroids. They’re not the same, and they don’t work the same way-but together, they’re the backbone of treatment for millions with asthma and COPD. Most people get them in an inhaler, but if you don’t know which one does what, or when to use them, you’re not getting the full benefit. This isn’t about taking pills-it’s about timing, technique, and understanding exactly how these drugs change what’s happening inside your lungs.
How Bronchodilators Open Your Airways
Bronchodilators don’t fix inflammation. They don’t calm down your immune system. What they do is simple: they relax the muscles that squeeze your airways shut. Think of them as a doorstop for your breathing passages. When these muscles tighten-usually because of triggers like cold air, allergens, or exercise-your lungs feel like they’re closing in. Bronchodilators step in and force them open.
There are two main types. The first are beta-2 agonists, like albuterol (also called salbutamol). These work by attaching to receptors in the airway muscles, triggering a chemical chain reaction that tells the muscle to loosen up. You’ll feel the difference in 15 to 20 minutes. That’s why albuterol inhalers are blue-they’re your rescue inhaler. If you’re wheezing or short of breath, one puff can get you back on your feet.
The second type is anticholinergics, like ipratropium and tiotropium. These block a different signal-acetylcholine-that tells your airways to tighten. Ipratropium kicks in around the same time as albuterol and lasts about 4 to 6 hours. Tiotropium, the long-acting version, lasts a full day. These are often used in COPD, but they’re also combined with beta-2 agonists for people who need extra help.
Short-acting bronchodilators (SABAs) are meant for quick relief. Long-acting ones (LABAs) like salmeterol or formoterol are not for emergencies. They take 30 minutes to start working and last 12 hours or more. But here’s the catch: LABAs alone can be dangerous. Studies show using them without an anti-inflammatory drug increases the risk of severe asthma attacks-and even death. That’s why they’re never prescribed by themselves for asthma.
How Corticosteroids Quiet the Inflammation
If bronchodilators are the doorstop, corticosteroids are the peacekeepers. They don’t open your airways. They stop the swelling that keeps them narrowing in the first place. Think of it like this: your airways are like a garden hose. Bronchodilators stretch the hose open. Corticosteroids stop the gunk inside from building up and clogging it.
Inhaled corticosteroids (ICS) like fluticasone, budesonide, and beclomethasone work at the genetic level. They slip into cells in your airways and turn down the volume on over 100 inflammatory genes. That means fewer immune cells showing up to cause damage, less mucus production, and less swelling. But they don’t work fast. You won’t feel better after one puff. It takes days-sometimes weeks-of daily use before your lungs start to calm down.
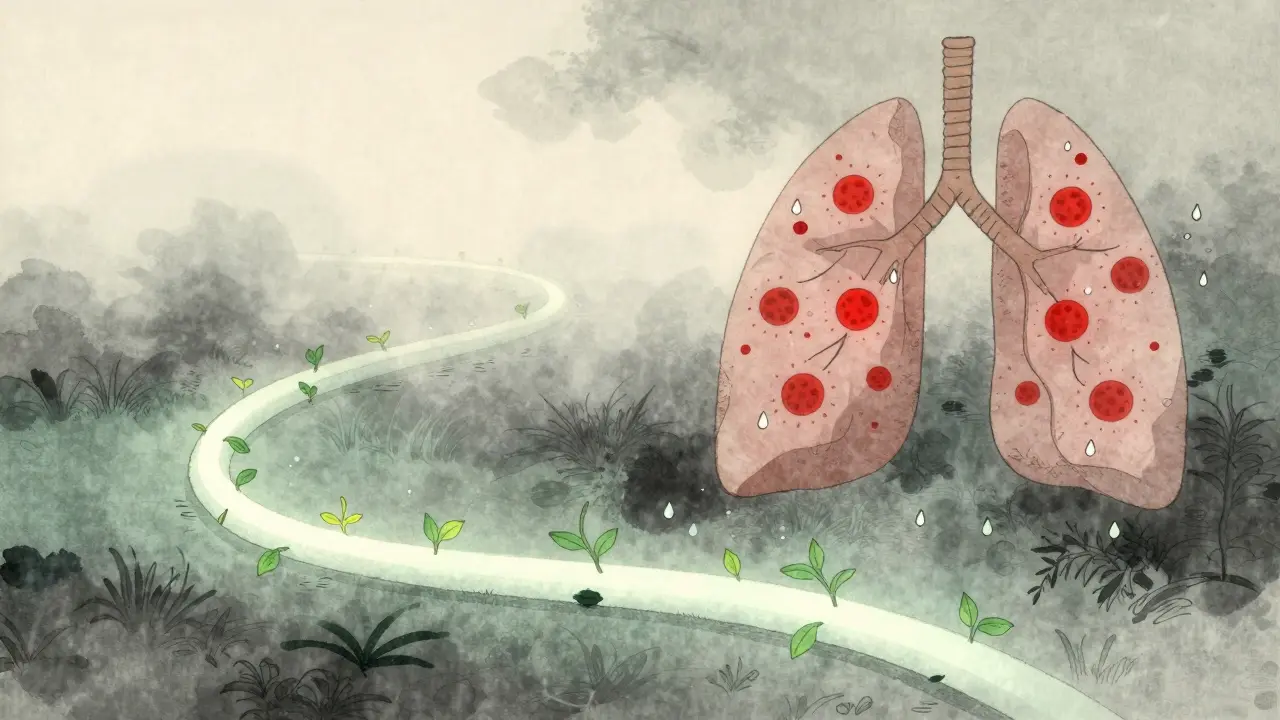
This is why so many people stop using them. They feel fine one day, so they skip the inhaler. Then, two weeks later, they’re back in the ER. Corticosteroids aren’t for emergencies. They’re for prevention. Regular use cuts asthma flare-ups by 30% to 60%, according to the American College of Allergy, Asthma & Immunology. For COPD patients with frequent flare-ups, they reduce hospital visits by nearly half.
But they’re not side-effect free. About 5% to 10% of users get oral thrush-a fungal infection that makes the mouth feel coated and sore. It’s not dangerous, but it’s annoying. The fix? Rinse your mouth with water after every puff. Don’t swallow it. Spit it out. That simple step cuts thrush risk by more than half. Some users also report hoarseness or a scratchy throat. Again, rinsing helps. And yes, long-term high doses can slightly raise the risk of pneumonia in older adults with COPD. But for most people, the benefits far outweigh the risks.
Why You Need Both-and How to Use Them Right
Here’s the biggest mistake most people make: using their corticosteroid inhaler before their bronchodilator. That’s like trying to paint a wall before you fix the holes. If your airways are tight, the corticosteroid can’t reach deep into the lungs. It sticks in your throat or the big airways. You’re wasting most of the dose.
The right order is simple:
- Use your bronchodilator first (usually the blue inhaler).
- Wait 5 minutes. Let the muscles relax fully.
- Then use your corticosteroid (usually the brown or white one).
This isn’t just advice-it’s backed by science. A 2023 Cleveland Clinic study showed that patients who followed this sequence had 40% more medication reaching the small airways. One Reddit user, who’d been using asthma meds for 12 years, said, “I didn’t realize how much better my breathing was until I started waiting 5 minutes between inhalers.”
Combination inhalers-like Advair (fluticasone/salmeterol) or Symbicort (budesonide/formoterol)-make this easier. They deliver both drugs in one puff. Symbicort is even approved for as-needed use in mild asthma now, thanks to studies showing it cuts severe flare-ups by 64% compared to using albuterol alone. That’s a game-changer. It means you’re getting both immediate relief and anti-inflammatory action in one step.
What Happens When You Get It Wrong
Skipping your corticosteroid? You’re treating symptoms, not the disease. You might feel okay for a while-but the inflammation keeps building. Over time, your lungs get more sensitive. You start needing your rescue inhaler more often. Then, one day, it doesn’t work as well. That’s not your fault-it’s the medicine’s. Chronic overuse of SABAs can cause your body to stop responding to them. Some heavy users lose up to 50% of the drug’s effect.
Using your rescue inhaler 10 or 15 times a week? That’s a red flag. The American Lung Association says most people should need it no more than 2 to 3 times a week. If you’re using it more, your asthma isn’t controlled. You need to talk to your doctor about adding or adjusting your corticosteroid.
And if you don’t rinse after using your corticosteroid? You’re inviting thrush. A 2022 Mayo Clinic survey found 42% of users had at least one episode of oral thrush-almost all of them were people who skipped rinsing. It’s preventable. It’s simple. But it’s ignored.
Getting the Most Out of Your Inhaler
Even if you know what to do, if you don’t use the inhaler right, it won’t work. Studies show only 31% of people use inhalers correctly without training. That’s why your doctor or pharmacist should watch you use it-twice. Here’s what matters:
- Slow, deep breath in: Press the inhaler and breathe in slowly over 3 to 5 seconds. Don’t just puff and gasp.
- Hold your breath: After inhaling, hold it for 10 seconds. That lets the medicine settle.
- Use a spacer: If you’re struggling with timing, a spacer (a plastic tube that attaches to your inhaler) can boost delivery by 70%. It’s cheap, reusable, and works with almost all inhalers.
- Check your technique: Every 6 months, ask your provider to watch you again. Technique slips over time.
Spacers are especially helpful for kids and older adults. They make it harder to mess up. And if you’re using a dry powder inhaler (DPI), you need a fast, strong inhale-not a slow one. Each device is different. Always read the instructions that come with yours.

What’s New and What’s Coming
The field is changing fast. In 2023, the FDA approved Airsupra, the first as-needed inhaler that combines albuterol and budesonide. It’s designed for people with mild asthma who want to ditch the blue inhaler-only approach. Early data shows it cuts severe attacks by 60% compared to albuterol alone.
Also, the GINA 2023 guidelines now recommend as-needed low-dose budesonide-formoterol (Symbicort) as the first-line treatment for mild asthma. That’s a huge shift. It means you’re not just treating symptoms-you’re preventing damage from day one.
Future tools are getting smarter. FeNO testing (measuring nitric oxide in your breath) is now recommended for 70% of asthma patients to help doctors fine-tune corticosteroid doses. It’s non-invasive, quick, and tells your doctor if inflammation is still active-even if you feel fine.
And yes, the environment is being considered. A single albuterol inhaler has the same carbon footprint as driving 300 miles. That’s why manufacturers are shifting toward dry powder inhalers, which don’t use propellants. They now make up 45% of new inhaler launches since 2020.
Final Thoughts: It’s Not Magic, It’s Mechanics
Bronchodilators and corticosteroids aren’t cure-alls. They don’t reverse lung damage. But they stop it from getting worse. They let you live without constant wheezing, without panic attacks over breathlessness, without ER visits. The key isn’t just taking them-it’s taking them right. Use the bronchodilator first. Wait five minutes. Then use the corticosteroid. Rinse your mouth. Use a spacer if you need it. And if you’re using your rescue inhaler more than twice a week, it’s time to talk to your doctor.
This isn’t about being perfect. It’s about being consistent. Small habits-like rinsing after inhalers or waiting five minutes-add up to big changes in how you breathe. And that’s the whole point.
Can I use my bronchodilator every day?
Short-acting bronchodilators (like albuterol) are meant for emergencies, not daily use. If you’re using them more than 2 to 3 times a week, your asthma isn’t controlled. You likely need a daily corticosteroid inhaler. Long-acting bronchodilators (LABAs) are safe for daily use-but only when combined with a corticosteroid. Never use a LABA alone.
Why do I need to rinse my mouth after using a corticosteroid inhaler?
Corticosteroids can leave a small amount of medicine in your mouth and throat. This can cause oral thrush, a fungal infection that leads to white patches, soreness, or a bad taste. Rinsing with water and spitting it out removes the residue and cuts your risk of infection by more than half. It’s a simple step that prevents a common and annoying side effect.
Is it okay to switch from separate inhalers to a combination inhaler?
Yes, and many people benefit from it. Combination inhalers like Advair or Symbicort simplify your routine, reduce the chance of mixing up doses, and ensure you get both medications at the right time. Studies show they improve adherence and reduce flare-ups. But don’t switch without talking to your doctor. They’ll check if the dose is right for your condition.
Do corticosteroids weaken my immune system?
Inhaled corticosteroids have very little effect on your overall immune system because they’re delivered directly to the lungs. Only a tiny amount enters your bloodstream. This is very different from oral steroids (like prednisone), which can weaken immunity. The main local side effect is thrush-not systemic immune suppression. But long-term, high doses may slightly raise pneumonia risk in older adults with COPD, which is why doctors monitor this closely.
What should I do if my inhaler stops working as well as it used to?
If your rescue inhaler isn’t relieving symptoms like it used to, it’s a warning sign. You might be overusing it, which can cause your body to become less responsive. Or your inflammation may have worsened. Either way, don’t increase the dose. Call your doctor. You may need a corticosteroid added or adjusted, or a switch to a combination inhaler. Ignoring this can lead to a serious flare-up.
