
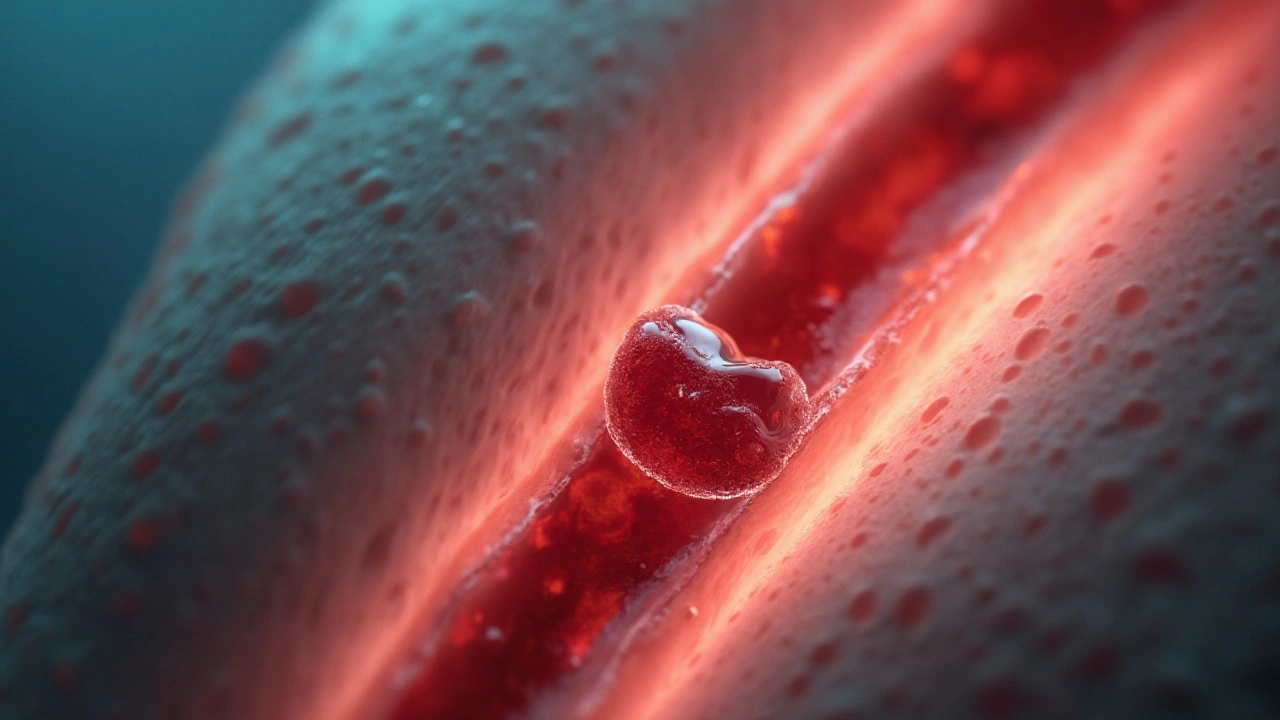
Blood clot is a gelatinous mass of fibrin and platelets that can obstruct veins or arteries. When a clot blocks a deep vein in the leg it’s called a deep vein thrombosis (DVT), and if that clot travels to the lungs it becomes a pulmonary embolism (PE). Blood clot risk spikes when the body's coagulation system is out of balance - and thyroid hormones play a surprisingly big part in that balance.
Quick Take
- Both hyper‑ and hypothyroidism can tip the coagulation cascade toward clotting.
- Autoimmune thyroiditis (Hashimoto) and Graves disease increase clot‑promoting antibodies.
- Genetic factors like Factor V Leiden magnify the danger when combined with thyroid imbalance.
- Regular monitoring of TSH, free T4, and platelet counts helps catch problems early.
- Lifestyle tweaks - weight control, movement, and adequate vitaminK - lower the odds of DVT and PE.
Why Thyroid Hormones Matter for Blood Clotting
The thyroid releases two main hormones, triiodothyronine (T3) and thyroxine (T4). They regulate metabolism, but they also influence the liver’s production of clotting factors (II, VII, IX, X) and the breakdown of fibrin through the fibrinolytic pathway. In hyperthyroidism, elevated T3 accelerates the synthesis of these factors, shortening clotting time and increasing platelet activation. In hypothyroidism, reduced metabolic rate slows the clearance of clotting proteins, leading to a pro‑thrombotic state despite lower platelet reactivity.
Think of the coagulation system as a seesaw. Thyroid hormones add weight to one side - too much or too little - and the balance tilts toward clot formation. Studies from the British Thyroid Association (2022) show a 1.7‑fold rise in DVT incidence among untreated hyperthyroid patients compared with euthyroid controls.
Who’s Most Vulnerable?
Risk isn’t uniform. Several overlapping factors raise the odds of a clot when thyroid disease is present:
- Autoimmune thyroiditis (Hashimoto) - chronic inflammation creates antiphospholipid antibodies that directly promote clotting.
- Graves disease - high thyroid‑stimulating immunoglobulins correlate with elevated fibrinogen levels.
- Genetic thrombophilias (e.g., Factor V Leiden) - the mutation alone raises clot risk; combined with thyroid imbalance the risk doubles.
- Age over 60, obesity, immobility (post‑surgery, long‑haul flights) - traditional DVT triggers that become more potent under hormonal dysregulation.
- Medications such as oral contraceptives or hormone replacement therapy - they add estrogen‑driven clotting pressure on top of thyroid effects.
Comparing Thyroid Conditions and Their Effect on Coagulation
| Condition | Typical Hormone Profile (TSH / Free T4) | Clotting Tendency |
|---|---|---|
| Hyperthyroidism | Low TSH, High Free T4 | Elevated (↑ clotting factor synthesis, ↑ platelet activation) |
| Hypothyroidism | High TSH, Low Free T4 | Elevated (↓ clearance of factors, ↑ fibrinogen) |
| Euthyroid (normal) | Normal TSH, Normal Free T4 | Baseline (balanced coagulation) |
| Autoimmune thyroiditis (Hashimoto) | Variable TSH, Variable Free T4 | Elevated (antiphospholipid antibodies) |
| Graves disease | Low TSH, High Free T4 | Elevated (↑ fibrinogen, inflammatory cytokines) |
Practical Steps to Lower the Risk
Knowing the link is only half the battle. Here’s a roadmap that patients and clinicians can follow:
- Screen thyroid function at least once a year for anyone with a personal or family history of clotting disorders.
- If TSH is abnormal, repeat testing in 4‑6 weeks and consider a full panel (Free T3, Free T4, anti‑TPO, TRAb).
- Check coagulation markers - PT/INR, aPTT, fibrinogen, D‑dimer - especially before surgery or if the patient reports leg swelling.
- When a thyroid disorder is confirmed, aim for euthyroid status using the lowest effective dose of antithyroid drugs, levothyroxine, or radioactive iodine.
- For hyperthyroidism, beta‑blockers can dampen platelet activation while awaiting definitive therapy.
- Consider prophylactic anticoagulation (low‑dose aspirin or a direct oral anticoagulant) if the patient has an additional high‑risk factor such as Factor V Leiden.
- Risk‑benefit discussion is essential - bleeding risk rises concurrently.
- Lifestyle tweaks:
- Maintain a healthy weight (BMI <25) - adipose tissue produces pro‑inflammatory cytokines that aggravate clotting.
- Move every 2 hours during long trips - simple calf‑pump exercises cut DVT odds by ~30%.
- Eat vitaminK‑rich foods (leafy greens) in moderation; they support normal clotting factor synthesis without causing excess clotting.
Related Concepts You Might Explore Next
Understanding thyroid‑related clot risk opens doors to a broader health picture. Readers often want to dive deeper into:
- Cardiovascular disease - how thyroid hormones affect cholesterol and heart rhythm.
- Endocrine disorders - interactions between adrenal, pituitary, and thyroid axes.
- Anticoagulant therapy - choosing between warfarin, DOACs, and aspirin for thyroid patients.
- Thyroid surgery recovery - DVT prevention protocols after thyroidectomy.
- Genetic thrombophilia testing - when to order Factor V Leiden or prothrombin gene analysis.
These topics sit just a click away and help round out a comprehensive plan for anyone juggling hormone health and clot prevention.
Checklist: Managing Blood Clot Risk with Thyroid Disorders
- ✅ Annual thyroid panel (TSH, Free T4, Free T3)
- ✅ Baseline coagulation screen if you have a known clotting mutation
- ✅ Keep a symptom diary - note leg swelling, chest pain, shortness of breath
- ✅ Discuss prophylactic anticoagulation when multiple risk factors coexist
- ✅ Prioritize movement and weight management
- ✅ Review medication list for estrogen‑containing drugs and adjust if needed
Frequently Asked Questions
Can hyperthyroidism cause a blood clot?
Yes. Excess thyroid hormone speeds up the liver’s production of clotting factors and heightens platelet stickiness, which together raise the chance of DVT and pulmonary embolism.
Is hypothyroidism also a risk factor for clotting?
It is. Low thyroid activity slows the breakdown of clotting proteins, leading to higher fibrinogen levels and a sluggish fibrinolytic system, both of which favor clot formation.
Should I be screened for clotting disorders if I have Hashimoto’s?
Screening is advisable if you have additional risk factors such as a family history of thrombosis, obesity, or prolonged immobility. A simple panel checking antiphospholipid antibodies and basic coagulation times can catch early problems.
Can taking levothyroxine increase my clot risk?
When dosed correctly to achieve a normal TSH, levothyroxine does not raise clot risk. Over‑replacement, however, can mimic hyperthyroid effects and should be avoided.
Do oral contraceptives add danger for someone with a thyroid disorder?
Yes. Estrogen increases clotting factor production, and when combined with thyroid‑induced pro‑coagulant changes the overall risk can be additive. Discuss alternative contraception with your doctor.
What lifestyle habits are most effective at reducing clot risk?
Regular aerobic activity, maintaining a healthy weight, staying hydrated, and moving the legs every couple of hours during long travel are the top evidence‑backed measures. Including leafy greens for vitaminK and limiting smoking also help.
Is a low‑dose aspirin enough to prevent clots if I have Graves disease?
Aspirin can be useful for mild risk, but many clinicians prefer a direct oral anticoagulant for patients with multiple risk factors. The decision must weigh bleeding risk, kidney function, and personal preferences.

20 Comments
Oh great, another thyroid‑clot thriller!!!
One must first acknowledge the ontological interplay between endocrine dysregulation and hemostatic equilibrium, a nuance often eclipsed by simplistic clinical heuristics. The hyperactive thyrotropic axis precipitates a cascade of hepatic transcriptional upregulation, thereby augmenting the synthesis of pro‑coagulant factors II, VII, IX, and X. Concurrently, the elevated metabolic rate enhances platelet reactivity through increased adrenergic tone, fostering a pro‑thrombotic environment. Conversely, hypothyroid states decelerate proteolytic clearance mechanisms, resulting in an accumulation of fibrinogen and plasma clotting proteins. The net effect is a biphasic risk model wherein both hormonal excess and deficiency tilt the coagulation seesaw toward thrombosis. Autoimmune thyroiditis introduces antiphospholipid antibodies, engendering an additional immunologic conduit to clot formation. Graves disease, via stimulating immunoglobulins, augments inflammatory cytokine release, further potentiating fibrinogen synthesis. Genetic predispositions such as Factor V Leiden compound these hormonal perturbations, effectively doubling the thrombotic propensity when co‑existent. Clinical surveillance should therefore integrate periodic assessment of TSH, free T4, and platelet indices alongside conventional coagulation panels. Therapeutic stratagems ought to prioritize restoration of euthyroidism, employing the minimal effective dose of antithyroid agents or levothyroxine. In selected high‑risk cohorts, low‑dose aspirin or direct oral anticoagulants may be justified, albeit with vigilant monitoring for hemorrhagic complications. Lifestyle interventions-weight optimization, regular ambulation, and adequate vitamin K intake-serve as adjunctive measures to attenuate venous stasis. Pre‑operative evaluation must be meticulous, with peri‑operative anticoagulation tailored to the individual's endocrine and hematologic profile. Finally, patient education regarding symptomatology of deep vein thrombosis and pulmonary embolism is indispensable for early detection and intervention. Thus, the confluence of thyroid pathology and coagulation dynamics mandates a multidisciplinary approach, bridging endocrinology, hematology, and primary care.
Regular thyroid checks can spot imbalances early, and tweaking meds can keep you in the sweet spot. Pair that with a simple walk each day and you’re already lowering clot risk.
Totally agree, and don’t forget to stay hydrated-dehydration can make the blood a bit stickier, especially if your thyroid’s off.
yeah but like the article forgets that many patients cant afford regular labs, so all this "watch your TSH" advice is kinda useless for low‑income folks.
The discourse overlooks the fact that not all hyperthyroid patients develop coagulopathies; the correlation is not universally deterministic.
😊 That's a fair point! Still, even a modest risk increase warrants vigilance, especially for those with other factors.
What they don't tell you is that big pharma is secretly pushing thyroid meds to keep us hooked on lifelong anticoagulants!!!
Think about the hidden agenda!!!
Everything is connected!!!
Honestly, that sounds a bit over the top, but staying active is still the best low‑cost move.
Wow, the drama in this thread is unreal!!!
People act like a simple thyroid test is the end‑all be‑all, when in reality it's just one piece of a massive puzzle!!!
Stop the hysteria!!!
Maybe, but the data does show a noticeable uptick in DVT cases among untreated hyperthyroid patients.
Let’s keep it friendly: sharing reliable sources helps everyone stay informed without the noise.
i think the article could've added a link to the British Thyroid Association study for quick reference.
Great effort on the overview! A little more emphasis on patient education would round it out nicely.
From a philosophical standpoint, the interplay between endocrine function and hemostasis underscores the intricate balance inherent in human physiology, reminding us that medical interventions must be approached with humility and rigor.
Check your punctuation; the article missed commas in several lists-clarity matters!
Of course the western meds are the problem-our own bodies know best! 😊
Honestly, reading this feels like wading through a sea of medical jargon that only specialists would love. The author tries to be comprehensive, but the sheer volume of technical terms can overwhelm a lay reader. Still, the core message-that thyroid health influences clot risk-is valuable. If they could break it down into simpler bullet points, we'd all benefit.
Good points, and adding a quick “what to ask your doctor” checklist would be helpful.
Nice summary-just remember, keep your thyroid meds on point and stay active.