SSRI Bleeding Risk Calculator
Your Risk Assessment
This calculator estimates your bleeding risk based on your medications and health factors. It's designed to help you discuss safer options with your doctor.
When you take an SSRI for depression or anxiety, you’re not just changing your mood-you’re affecting how your blood clots. It’s not something most people think about, but the same mechanism that lifts your spirits can also make you bleed more easily. This isn’t rare. It’s built into the biology of these drugs. And if you’re on blood thinners, older, or have a history of stomach issues, this isn’t just a footnote-it’s a real risk.
How SSRIs Stop Serotonin From Doing Its Job
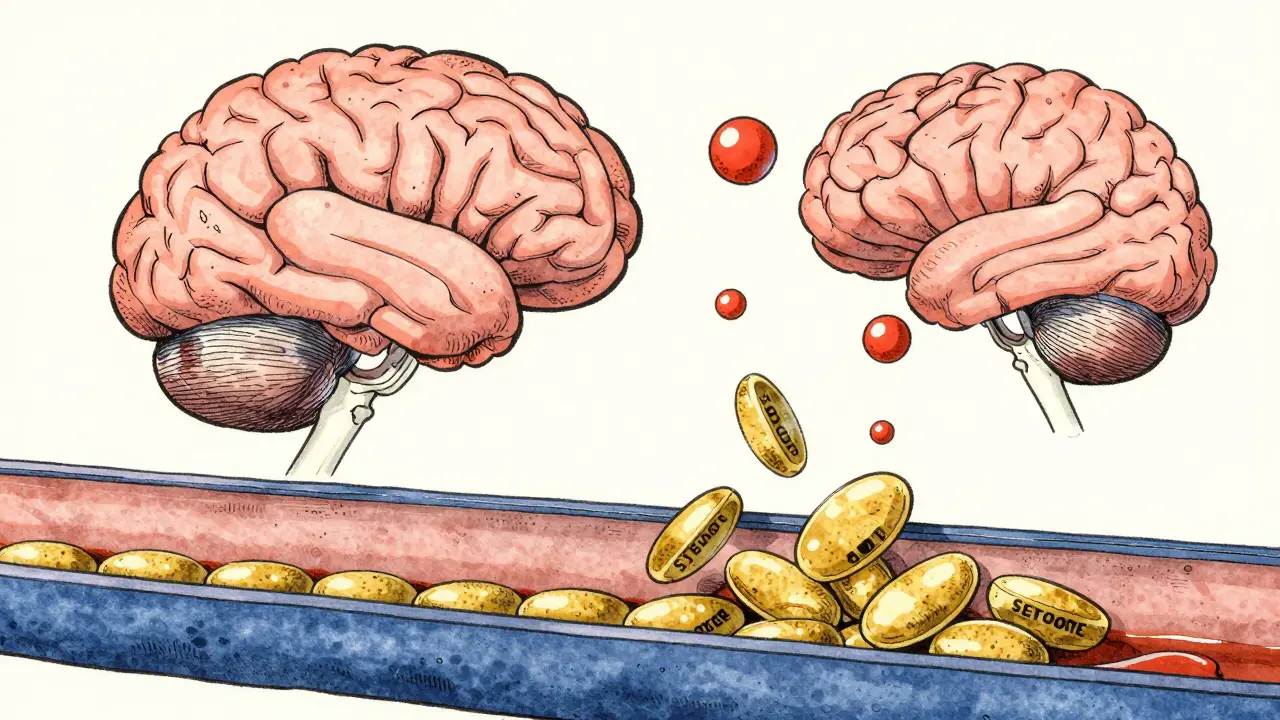
SSRIs like sertraline, fluoxetine, and paroxetine work by blocking the serotonin transporter, a protein that pulls serotonin back into brain cells after it’s released. More serotonin in the space between neurons means better mood regulation. But here’s the catch: platelets-the tiny blood cells that help stop bleeding-also use that same transporter. In fact, 99% of the body’s serotonin lives in platelets, not the brain.
When SSRIs block serotonin uptake in platelets, those cells can’t store enough of it. And serotonin isn’t just a mood chemical-it’s a key signal for platelets to stick together at injury sites. Without it, they don’t clump as effectively. Studies show that people taking paroxetine can lose over 80% of their platelet serotonin. That’s not a small drop. It’s enough to slow down clotting, sometimes dramatically.
Not All SSRIs Are Created Equal
Some SSRIs are much stronger at blocking serotonin uptake than others. This matters because the tighter the binding, the higher the bleeding risk. Paroxetine has the strongest grip on the serotonin transporter (Ki=0.17nM), followed by fluvoxamine. Sertraline and citalopram? They’re weaker. That’s why paroxetine users are 40-50% more likely to have upper GI bleeding than those on other antidepressants, according to FDA adverse event data.
Real-world reports back this up. On Reddit, users on paroxetine were nearly twice as likely to report unexplained bruising or prolonged bleeding after minor cuts compared to those on sertraline. Drugs.com user reviews show 18.7% of paroxetine users reported easy bruising-nearly double the rate of sertraline users (9.2%). It’s not just anecdotal. A 2024 meta-analysis in JAMA Network Open found that combining SSRIs with blood thinners like warfarin increased major bleeding risk by 35%.
When SSRIs and Other Drugs Collide
The biggest danger isn’t SSRIs alone-it’s what they’re taken with. NSAIDs like ibuprofen or naproxen already irritate the stomach lining and reduce platelet function. When you add an SSRI on top, the bleeding risk jumps 4.5 times, according to a 2013 study. That’s why doctors often warn against mixing them.
Anticoagulants like warfarin or apixaban are another red flag. The combination doesn’t just add risk-it multiplies it. In patients on both an SSRI and an oral anticoagulant, the chance of serious bleeding is significantly higher than with either drug alone. That’s why electronic health records now flag these combinations. One 2021 study of 147 U.S. hospitals showed that automated alerts cut SSRI-anticoagulant prescriptions by over 22%.
But it’s not all doom and gloom. A 2023 study of heart patients undergoing stent placement found no increased bleeding in those taking SSRIs-even when they were also on powerful antiplatelet drugs like ticagrelor. Why? Because modern antiplatelet therapy is so strong that the added effect of SSRIs gets drowned out. Context matters. Your overall risk depends on what else you’re taking, your age, and your health history.

Who’s Most at Risk?
You’re more likely to have problems if:
- You’re over 65
- You’ve had a stomach ulcer or GI bleed before
- You’re on blood thinners, NSAIDs, or antiplatelet drugs
- You have kidney or liver disease
- You drink alcohol regularly
The HAS-BLED score is a simple tool doctors use to measure this. It checks for Hypertension, Abnormal kidney/liver function, Stroke history, Bleeding history, Labile INR (if on warfarin), Elderly age, and Drugs/alcohol use. A score of 3 or higher means high risk-and that’s when you should talk about alternatives.
What to Do If You’re on an SSRI
Don’t stop your medication without talking to your doctor. Untreated depression carries its own risks-higher heart disease, worse recovery from surgery, even increased death rates. But you can make smarter choices.
If you’re at higher risk for bleeding:
- Ask about switching to sertraline or citalopram-they’re safer bets
- Avoid NSAIDs. Use acetaminophen instead for pain
- Tell every doctor you see that you’re on an SSRI, especially before surgery or dental work
- Consider stopping the SSRI 5-7 days before elective procedures with high bleeding risk (like colonoscopies or tooth extractions)
For major surgeries like heart operations, guidelines say to keep SSRIs going. The risk of depression relapse is too high. But for minor procedures? It’s worth discussing.

Signs You Might Be Bleeding Too Much
Most bleeding from SSRIs is mild-more bruising, longer nosebleeds, heavier periods. But watch for these red flags:
- Black, tarry stools (sign of upper GI bleeding)
- Vomiting blood or material that looks like coffee grounds
- Unexplained large bruises without injury
- Prolonged bleeding from cuts or gums
- Headaches, dizziness, or weakness that come on suddenly (possible internal bleeding)
If you see any of these, get help immediately. Don’t wait.
What’s Changing in 2025?
Doctors are starting to look beyond just which SSRI you’re on. New research shows your genes matter too. A variation in the serotonin transporter gene (5-HTTLPR) can make you 2.3 times more likely to bleed on SSRIs if you have the S/S genotype. Genetic testing for this isn’t routine yet-but it’s coming. The European Medicines Agency is reviewing whether to add genetic risk info to SSRI labels by late 2025.
Another promising idea? Platelet-rich plasma (PRP) infusions. A 2023 study showed PRP cut bleeding time by over 40% in SSRI patients before surgery. It’s experimental, but it shows we’re moving toward solutions, not just warnings.
The Bottom Line
SSRIs are not dangerous for most people. But they’re not harmless either. The link between serotonin, platelets, and bleeding is real, well-studied, and predictable. The key isn’t avoiding SSRIs-it’s matching the right drug to your risk profile.
If you’re young, healthy, and not on other blood-thinning meds, sertraline or escitalopram are low-risk choices. If you’re older, on warfarin, or have a history of ulcers, talk to your doctor about alternatives like bupropion or mirtazapine, which don’t affect platelets at all.
The goal isn’t to scare you off antidepressants. It’s to make sure you get the mental health care you need without unexpected complications. Bleeding risk is real-but it’s manageable. With the right info and the right drug, you can feel better without putting yourself at risk.
Do all SSRIs cause bleeding?
No. Not all SSRIs carry the same bleeding risk. Paroxetine and fluvoxamine are the strongest at blocking serotonin uptake in platelets, making them highest risk. Sertraline, citalopram, and escitalopram have weaker effects and are safer choices if bleeding risk is a concern.
Can I take ibuprofen with an SSRI?
It’s not recommended. Combining NSAIDs like ibuprofen with SSRIs increases bleeding risk by 4.5 times. Use acetaminophen (Tylenol) for pain relief instead. Always check with your doctor before mixing any over-the-counter meds with your antidepressant.
Should I stop my SSRI before surgery?
For minor procedures with high bleeding risk-like dental work or colonoscopies-your doctor may advise stopping the SSRI 5-7 days beforehand. For major surgeries like heart operations, guidelines say to keep taking it. Depression relapse during recovery can be deadly. Always discuss this with your surgical team and psychiatrist.
Is there a genetic test for SSRI bleeding risk?
Yes, but it’s not routine yet. A gene variant called 5-HTTLPR affects how your body handles serotonin. People with the S/S genotype have 2.3 times higher bleeding risk on SSRIs. Research is advancing fast, and the European Medicines Agency may require this info on labels by late 2025.
What are safer alternatives to SSRIs for people at risk of bleeding?
Bupropion (Wellbutrin) and mirtazapine (Remeron) are two antidepressants that don’t affect platelet serotonin. They’re often recommended for people with bleeding risks, history of ulcers, or those on blood thinners. They work differently than SSRIs but can be just as effective for depression and anxiety.

9 Comments
man i was on paroxetine for a year and never thought about the bleeding thing till now. i got a nosebleed that lasted 20 mins after a sneeze and just thought i was dry as hell. guess i got lucky. switched to sertraline and no more weird bruises. ps: doc never mentioned this either lol
The pharmacodynamic profile of SSRIs with high affinity for the SERT transporter (Ki < 0.2 nM) induces significant platelet serotonin depletion, impairing secondary hemostasis. Paroxetine and fluvoxamine demonstrate the most pronounced effect due to their binding kinetics. Clinical correlation is well-documented in cohort studies with GI hemorrhage incidence rising by 40-50% in these cohorts. Avoid concurrent NSAID use-synergistic COX-1 inhibition exacerbates mucosal vulnerability. Sertraline and escitalopram remain first-line for patients with bleeding risk factors.
if you’re on blood thinners or older, just stick with sertraline. it’s the safest ssri for your blood. no need to overthink it. also skip ibuprofen-use tylenol instead. simple. my grandma’s on it and she’s 78 and still hiking. no issues.
People take these pills like candy and then act shocked when their body starts acting up. This isn’t a mystery. It’s biology. If you can’t even read the warning label, maybe you shouldn’t be on psychiatric meds at all. Stop blaming doctors. Take responsibility.
really interesting! i’m on sertraline and just had a tooth extraction last week-no bleeding issues. but my friend took paroxetine and bled for hours after a small cut. i’ll tell him to talk to his doc about switching. also, the genetic part? mind blown. i didn’t know our dna could affect this. thanks for sharing!
so now we’re gonna let big pharma tell us which antidepressant our bodies can handle? what’s next? a federal SSRI license? we’re in america, folks-take your meds, don’t whine about bruising. if you’re bleeding, maybe you’re just weak. or maybe you’re on too many pills. get off the welfare meds and grow a spine.
omg this is so important!! 🙌 i didn’t know SSRIs could do this!! i’ve been on citalopram for 3 years and just got a huge bruise on my thigh for no reason-now it makes sense!! i’m telling my doctor tomorrow!! also, PRP infusions?? sounds like sci-fi but i’m here for it 💉✨
so let me get this straight-you’re telling me the same drug that makes me stop crying at 3am also makes me bleed like a stuck pig? genius. thanks, science. guess i’ll just start wearing a diaper and carrying a first aid kit everywhere. 🙃
While I appreciate the clinical depth of this post, I must emphasize that the assumption that patients can autonomously switch SSRIs without psychiatric supervision is dangerously misleading. Depression relapse carries a 15-20% mortality risk in high-risk populations. The decision to alter pharmacotherapy must involve multidisciplinary coordination-including psychiatry, primary care, and pharmacy. The data supports risk stratification, not self-adjustment. Please consult your provider before any change.