When you stand up from a chair, your body should automatically adjust your blood pressure to keep you from feeling dizzy or fainting. But for people with autonomic neuropathy, that automatic system breaks down. Instead of stabilizing, blood pressure plummets-sometimes within seconds. At the same time, food sits in the stomach, bloating and nausea set in, and bowel movements become unpredictable. These aren’t random side effects. They’re direct results of damaged nerves that control the body’s invisible functions: heart rate, digestion, blood pressure, and more.
What Exactly Is Autonomic Neuropathy?
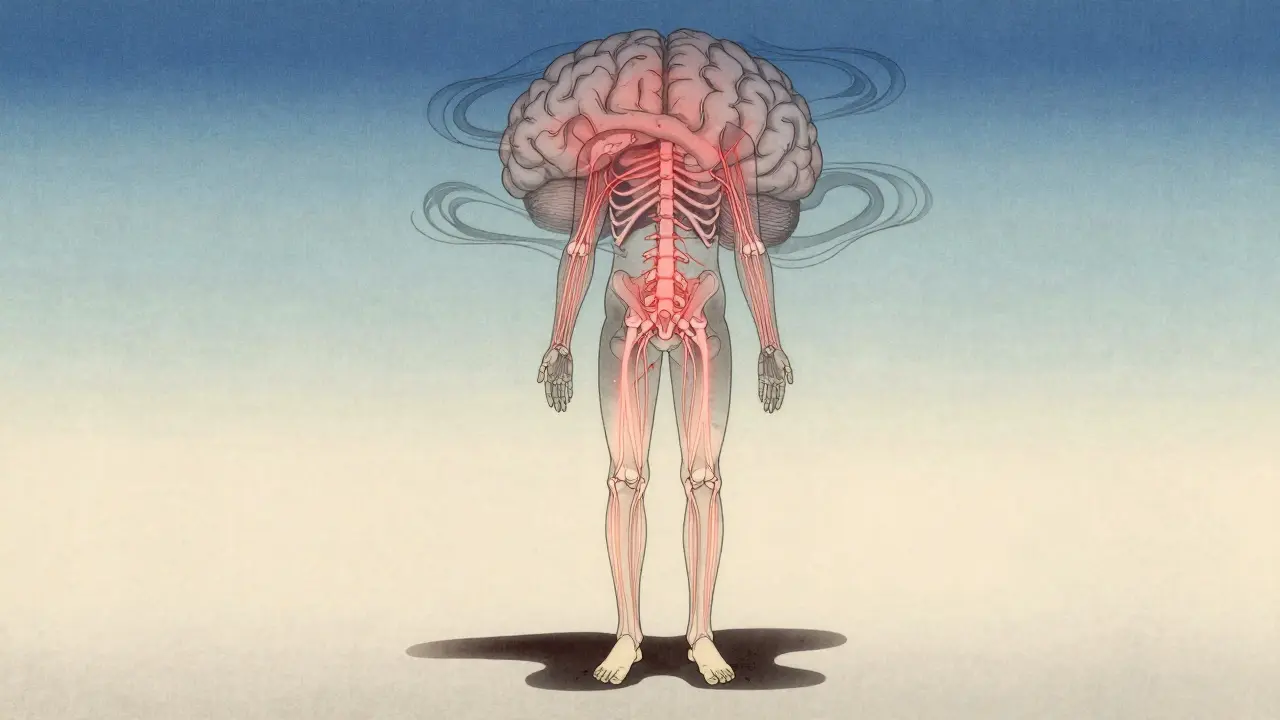
Autonomic neuropathy isn’t one disease-it’s a collection of symptoms caused by damage to the autonomic nervous system. This part of your nervous system runs in the background, managing everything you don’t think about: how fast your heart beats, how your stomach digests food, how your pupils react to light, and whether your blood vessels tighten or relax to maintain pressure. When these nerves get damaged, your body loses its ability to respond to changes-like standing up, eating a meal, or even staying warm.
Diabetes is the main cause, responsible for 85-90% of cases. High blood sugar over years slowly chews away at the tiny blood vessels that feed these nerves. But it’s not just diabetes. Chemotherapy, autoimmune diseases like Guillain-Barré, Parkinson’s, and even some viral infections can trigger it. The problem? Most people don’t realize they have it until symptoms become severe. In fact, doctors only catch about 30% of cases during routine visits.
Why Does Your Blood Pressure Crash When You Stand Up?
Standing up should be simple. Gravity pulls blood down into your legs. Your body responds by tightening blood vessels and speeding up your heart to keep blood flowing to your brain. In autonomic neuropathy, that signal doesn’t get through. The nerves that tell your blood vessels to squeeze don’t fire. Your heart doesn’t speed up fast enough. Blood pools in your lower body. Your brain gets less oxygen. And you feel lightheaded, blurry, or worse-you pass out.
This is called orthostatic hypotension. Doctors define it as a drop of at least 20 mmHg in systolic pressure or 10 mmHg in diastolic pressure within three minutes of standing. In real terms, that means your blood pressure might drop from 120/80 to 95/65 the moment you get up. For many, it happens daily. One study found that 68% of patients with confirmed autonomic neuropathy had systolic pressure below 90 mmHg during standing tests. Nearly half reported fainting or near-fainting episodes at least once a week.
Some people develop POTS instead-Postural Orthostatic Tachycardia Syndrome. Their blood pressure doesn’t drop much, but their heart races. A jump of 30 beats per minute or more within 10 minutes of standing is the hallmark. POTS affects 1-3 million Americans, mostly women between 15 and 50. It’s often misdiagnosed as anxiety or panic disorder. But the heart isn’t racing because you’re scared-it’s racing because the nervous system is broken.
What’s Going On in Your Stomach and Gut?
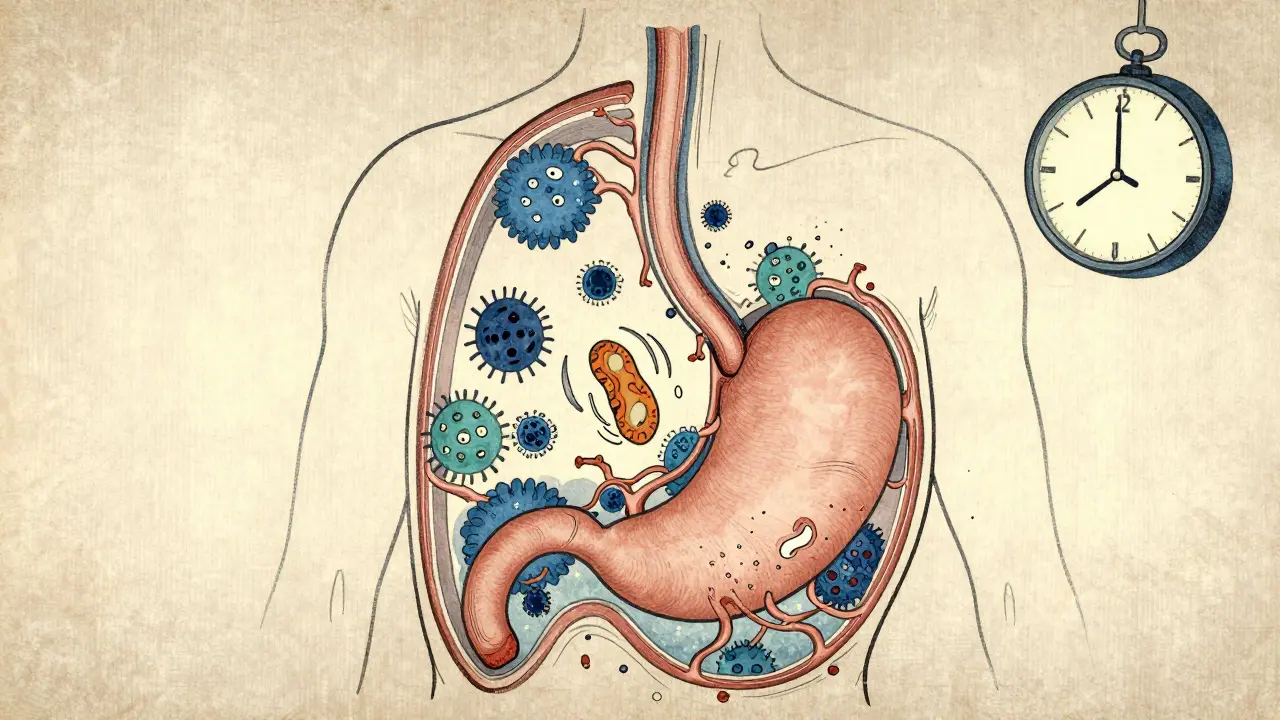
While blood pressure crashes, your digestive system is also falling apart. About one in three people with autonomic neuropathy develop gastroparesis-delayed stomach emptying. Food doesn’t move from your stomach to your intestines like it should. Instead, it sits there. You feel full after just a few bites. You vomit, often at night. Bloating becomes constant. One study found that 78% of gastroparesis patients with this condition had vomiting episodes at night.
Constipation is even more common, affecting 60% of patients. Bowel movements drop from the normal 4-5 times a week to just 1 or 2. Meanwhile, 25% deal with diarrhea-usually sudden, watery, and often at night. Some get both: constipation one day, diarrhea the next. This rollercoaster is called alternating bowel syndrome, and it’s a red flag for autonomic nerve damage.
Behind many of these GI symptoms is small intestinal bacterial overgrowth, or SIBO. When food sits too long in the gut, bacteria multiply. In autonomic neuropathy, 52% of patients with GI symptoms test positive for SIBO-compared to just 15% in healthy people. That’s why bloating, gas, and diarrhea don’t go away with diet changes alone. The problem isn’t just what you eat-it’s that your gut can’t move food properly.
How Do Doctors Diagnose This?
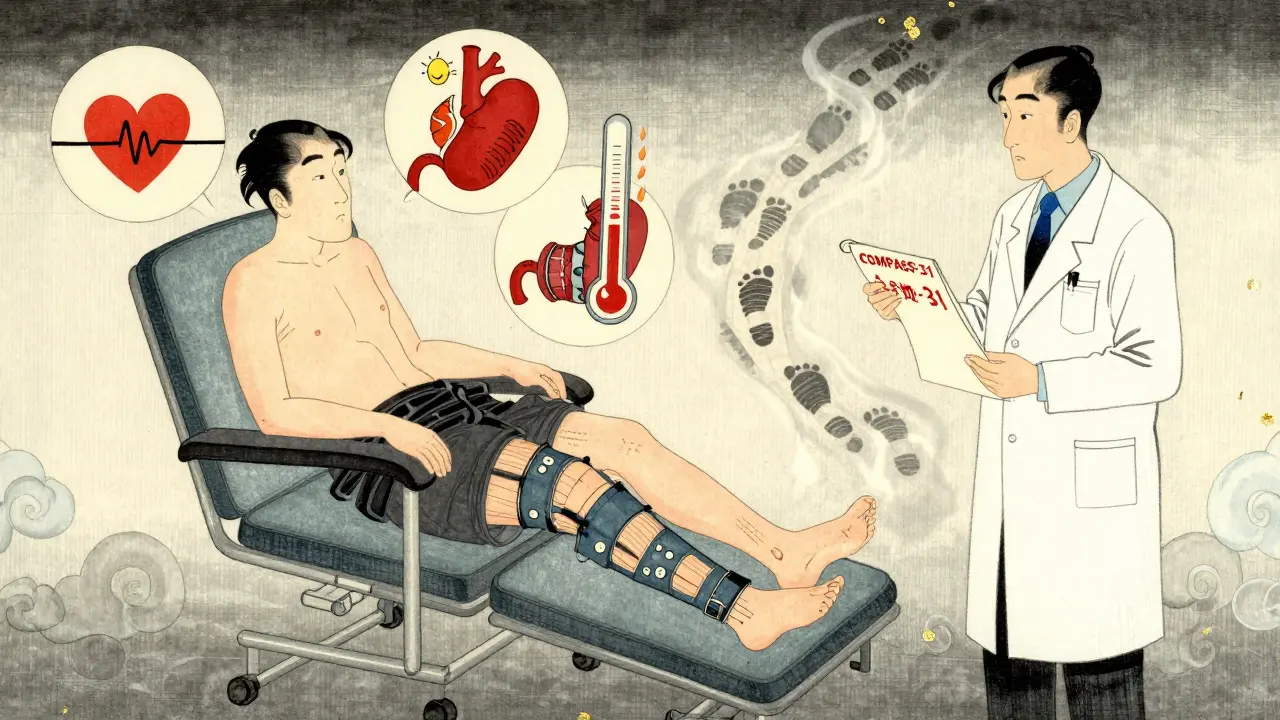
There’s no single blood test. Diagnosis relies on testing how your body responds to stress. The most common first step is the 10-minute active stand test. You lie down for five minutes, then stand up while your blood pressure and heart rate are monitored. A drop of 20 mmHg systolic or 10 mmHg diastolic confirms orthostatic hypotension.
Heart rate variability during deep breathing is another key test. Healthy people’s heart rate naturally rises when they inhale and falls when they exhale. In autonomic neuropathy, that variation disappears. The ratio of inhale to exhale heart rate drops below 1.1-a clear sign of nerve damage.
For gut issues, gastric emptying scintigraphy is the gold standard. You eat a meal with a harmless radioactive tracer, then an imaging scan tracks how long it takes to leave your stomach. If more than 10% is still there after four hours, you have gastroparesis. Newer tests like the wireless motility capsule are 92% accurate and don’t require radiation.
Doctors also use questionnaires like COMPASS-31, which scores symptoms from 0 to 100. A score above 30 means significant dysfunction. These tools help link how you feel to what’s actually happening in your nerves.
Treatment: What Actually Works?
There’s no cure, but there are ways to manage symptoms-and some work better than others.
For blood pressure drops, fludrocortisone helps by making your body hold onto more salt and water. It works for 60% of people, but 35% end up with high blood pressure when lying down-a dangerous trade-off. Midodrine tightens blood vessels and reduces symptoms in 70% of cases. But it must be taken at the right times-no doses after 6 p.m., or you’ll struggle to sleep because your blood pressure stays too high.
For POTS, ivabradine is a game-changer. It slows the heart without lowering blood pressure. In studies, it cuts heart rate by 15-25 beats per minute in 65% of users. No more racing heart when you stand up.
For gastroparesis, metoclopramide was once the go-to. But it carries a serious risk of permanent movement disorders after 12 weeks. Erythromycin works short-term but loses effectiveness fast. The newer option, pyridostigmine, improves symptoms in 55% of patients with fewer side effects. It’s becoming the first-line choice.
Non-drug approaches are just as important. Compression stockings (30-40 mmHg) reduce orthostatic symptoms by 35%. Abdominal compression garments help with bloating and nausea. Eating six small meals a day instead of three big ones cuts vomiting episodes in half. Cutting fat under 25 grams and fiber under 10 grams a day makes a huge difference. One patient on Reddit said: “The low-fat, low-residue diet cut my vomiting from five times a day to once every three days.”
What Patients Are Saying
Real people living with this condition share the same stories across forums. On Reddit’s r/dysautonomia, 82% say orthostatic symptoms are the most disabling. Many describe “brain fog” during dizzy spells-like their mind shuts down when their blood pressure drops. Over 70% wear compression garments daily. Nearly 90% avoid hot environments because heat makes symptoms worse.
For GI issues, 62% say their diet has ruined social life. Going out to eat? Too risky. Restaurants serve big meals, fatty foods, and high-fiber salads-all triggers. One user wrote: “I used to love brunch. Now I bring my own food.”
The biggest complaint? Delayed diagnosis. On average, people see three doctors over 4.7 years before getting the right answer. Many are told it’s anxiety, depression, or just “getting older.”
What’s Changing in 2026?
The field is moving fast. The American Diabetes Association now recommends annual autonomic screening for anyone with diabetes longer than seven years. That could catch 500,000 new cases each year. New guidelines are lowering the threshold for orthostatic hypotension-from a 20 mmHg drop to 15 mmHg-so we catch it earlier.
Blood tests for neurofilament light chain, a protein released when nerves are damaged, are now being tested as an early warning sign. It could replace invasive tests someday.
Fecal microbiota transplants (FMT) are being studied for gut symptoms. Early results show 40% improvement in GI quality of life after six months. That’s promising for people who’ve tried everything else.
But the reality remains grim. Severe autonomic neuropathy still cuts life expectancy by over eight years compared to diabetics without it. The nerves don’t heal. The damage is often permanent. That’s why early detection and aggressive symptom management aren’t just helpful-they’re life-saving.
Can autonomic neuropathy be reversed?
No, the nerve damage from autonomic neuropathy cannot be reversed. However, managing the underlying cause-like tightly controlling blood sugar in diabetes-can prevent further damage. Symptom treatments can significantly improve quality of life, but the nerves themselves don’t regenerate. Early diagnosis is critical to slow progression.
Is orthostatic hypotension the same as POTS?
No. Orthostatic hypotension means your blood pressure drops when you stand up. POTS means your heart rate spikes by 30 beats per minute or more, but your blood pressure stays stable. Both are forms of autonomic dysfunction, but they involve different nerve pathways. Some people have both. Others have only one.
Why do I feel dizzy even when I’m not standing?
Autonomic neuropathy affects more than just posture. Your body’s ability to regulate blood pressure during heat exposure, after meals, or even during emotional stress is impaired. Hot showers, eating a large meal, or sudden stress can trigger drops in blood pressure even while sitting or lying down. This is called non-orthostatic hypotension and is common in advanced cases.
Can diet alone fix gastroparesis symptoms?
Diet helps, but it rarely fixes it alone. Eating small, low-fat, low-fiber meals improves symptoms in 60% of patients, but most still need medication or other interventions. The problem isn’t just what you eat-it’s that your stomach can’t move food. Diet reduces the burden, but doesn’t fix the broken system.
How do I know if I have autonomic neuropathy and not just stress or anxiety?
Anxiety causes temporary symptoms. Autonomic neuropathy causes consistent, measurable dysfunction. If you have daily dizziness when standing, unexplained vomiting, constipation alternating with diarrhea, and heart racing without cause, and these symptoms persist for months, it’s not anxiety. Objective tests like the active stand test, heart rate variability, or gastric emptying scans can confirm it. If your symptoms match the pattern described here, ask your doctor for an autonomic evaluation.

2 Comments
It's wild how much our bodies just... work, until they don't. I never thought about how many things happen without me even noticing-like my blood vessels tightening when I stand up. It's not just about dizziness; it's like your body's silent orchestra gets muted, and suddenly you're lost in the noise.
Reading this made me realize how little we appreciate the invisible systems keeping us alive. We notice when we're sick, but never when we're perfectly fine. That’s the real tragedy here-most people won't know they're losing something until it's gone.
Bro, I’ve been living this for 5 years 😔
Compression socks = my new best friend. Also, I carry electrolyte packets everywhere. No more brunch dates, but at least I don’t pass out in Starbucks anymore. 🙏