
Carb Intake Calculator
Manage Your Side Effects
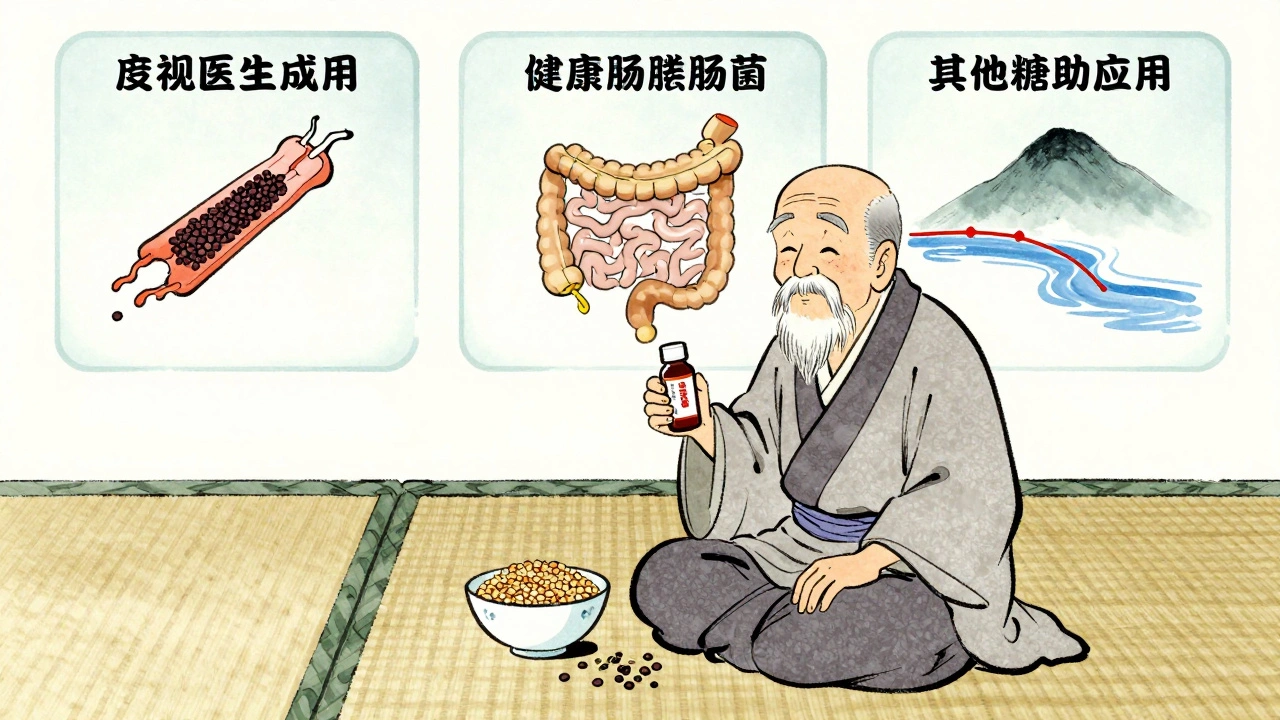
Based on article recommendations: Limit carbs to 30-45g per meal to reduce gas and bloating from alpha-glucosidase inhibitors. Enter your food portions below.
When you're managing Type 2 diabetes, the goal isn't just to lower blood sugar-it's to do it without making your daily life unbearable. That’s where alpha-glucosidase inhibitors come in. These drugs, like acarbose and miglitol, are designed to stop your body from breaking down carbs too fast after meals. That means fewer spikes in blood sugar. But there’s a catch: they turn your gut into a fermentation lab. The result? Gas, bloating, and diarrhea-often badly enough that people quit taking them.
Why These Drugs Cause So Much Gas
Alpha-glucosidase inhibitors don’t get absorbed into your bloodstream. Instead, they sit in your small intestine and block enzymes that normally break down complex carbs like bread, rice, and potatoes into simple sugars. That sounds good-until you realize what happens next. The undigested carbs don’t disappear. They travel straight to your colon, where your gut bacteria feast on them. That fermentation process produces hydrogen, methane, and carbon dioxide-aka, gas. And because those carbs pull water into your colon as they ferment, you get diarrhea and bloating too.
This isn’t a rare side effect. In the first month of treatment, up to 73% of people on acarbose report excessive flatulence, according to a 2020 meta-analysis. After six months, that number drops to about 25% as your gut microbiome slowly adjusts. But for many, those first few weeks feel like a daily battle. One user on Reddit said, “I had to stop after two weeks. The gas was so bad, I couldn’t leave the house.”
How Common Are These Side Effects?
Let’s be clear: these side effects aren’t just possible-they’re expected. Here’s what the data shows:
- Flatulence: 30-50% of users, up to 73% in early treatment
- Abdominal discomfort or bloating: 14-30%
- Diarrhea: 10-20%
Compare that to metformin, the most common diabetes drug. It causes nausea and vomiting in 20-30% of people, but rarely leads to the kind of lower GI distress you get with acarbose. GLP-1 agonists like semaglutide cause nausea in nearly half of users, but they don’t produce gas. SGLT2 inhibitors? Almost no GI side effects at all. So if you’re looking for a drug that won’t make you feel like a pressure cooker, alpha-glucosidase inhibitors aren’t the top pick.
Who Still Uses These Drugs Today?
Despite the side effects, they haven’t disappeared. In fact, they’re still prescribed-just not to everyone. They’re most often used for:
- People who can’t take metformin due to kidney issues
- Older adults (65+) where low blood sugar from other drugs is dangerous
- Patients who refuse or can’t afford injectables like GLP-1 agonists
- Those with very high post-meal blood sugar spikes
In the U.S., only 3.2% of diabetes prescriptions in 2023 were for acarbose or miglitol. But in China and India, where diets are high in rice and wheat, they’re far more common-used in over 10% of cases. Why? Because they work well on those kinds of meals. And at $15-$25 a month for generic acarbose, they’re cheap. That matters in places where newer drugs cost hundreds per month.

How to Reduce the Side Effects (Without Quitting)
If your doctor prescribed this drug and you’re struggling, don’t assume you have to suffer. There are proven ways to make it tolerable.
1. Start Low, Go Slow
Never start at 100 mg three times a day. That’s a recipe for disaster. The standard advice is to begin with 25 mg once a day-with your biggest meal. After a week, if you’re not too uncomfortable, add a second dose. Then, after another week, add the third. This slow ramp-up gives your gut time to adapt. Studies show this cuts discontinuation rates by nearly half.
2. Change Your Carbs
Not all carbs are created equal. The more refined your carbs, the worse the side effects. White bread, white rice, potatoes, sugary snacks? These are the worst. They’re broken down quickly, so when the enzyme blocker hits them, you get a huge amount of undigested sugar rushing to your colon.
Switch to:
- Whole grains (oats, barley, quinoa)
- Legumes (lentils, chickpeas, black beans)
- Non-starchy vegetables (broccoli, spinach, zucchini)
These digest slowly, so even if some carbs slip through, they don’t overwhelm your gut. Aim for 30-45 grams of carbs per meal. That’s about one slice of whole grain bread, half a cup of brown rice, and a big serving of veggies.
3. Avoid These Mistakes
- Don’t take Beano. It contains alpha-galactosidase, which breaks down the same carbs acarbose is trying to block. It can make your blood sugar spike.
- Don’t eat high-fat meals. Fat slows digestion, which means more carbs reach your colon. That worsens diarrhea.
- Don’t skip meals. These drugs only work if taken with food. If you skip a meal, you’re taking a drug with no purpose-and still getting side effects.
4. Use Simethicone for Gas
Simethicone (like Gas-X or Mylanta Gas) doesn’t stop the gas from forming, but it helps break up bubbles. Taking 125 mg before meals can reduce bloating and discomfort. It’s safe, over-the-counter, and doesn’t interfere with the drug.
5. Try Probiotics (New Evidence)
A 2023 clinical trial found that taking acarbose with a specific probiotic blend-Lactobacillus acidophilus and Bifidobacterium lactis-reduced gas severity by 35%. The probiotics didn’t block the drug’s effect. They just helped your gut handle the extra carbs better. Talk to your doctor about a quality, multi-strain probiotic. Don’t just grab any bottle off the shelf.
When to Consider Stopping
It’s okay to quit if it’s not working for you. About 15-20% of people stop within three months because the side effects are too much. That’s normal. But don’t quit without a plan. If you’re struggling:
- Ask your doctor about lowering the dose again
- Review your diet with a registered dietitian
- Give it 8-12 weeks-many people improve by then
If you’ve tried everything and it’s still unbearable, there are better options. SGLT2 inhibitors (like empagliflozin) have minimal GI side effects. GLP-1 agonists work better for weight loss and heart protection. Metformin is still the first choice for most. Alpha-glucosidase inhibitors are not a first-line drug for a reason.
What Success Looks Like
Some people do stick with it-and thrive. One user on Drugs.com wrote: “First month was hell. Gas, diarrhea, bloating. By month three, it was manageable. My post-meal sugars dropped from 220 to 160. Worth it.”
That’s the trade-off. You trade short-term discomfort for steady, predictable blood sugar control. No hypoglycemia. No weight gain. Just a quieter, more stable glucose curve after meals.
But here’s the truth: for most people, the discomfort outweighs the benefit. These drugs aren’t broken-they’re just outdated. Newer drugs do more with fewer side effects. But if you’re in a situation where other drugs aren’t safe or affordable, and you’re willing to manage the GI issues, alpha-glucosidase inhibitors can still play a role.
The key isn’t just taking the pill. It’s changing your diet, pacing your dose, and knowing this isn’t a life sentence. Your gut will adapt. Or you’ll find something better.
Do alpha-glucosidase inhibitors cause weight gain?
No. Unlike insulin or some other diabetes drugs, alpha-glucosidase inhibitors don’t cause weight gain. In fact, because they reduce how many calories your body absorbs from carbs, some people lose a small amount of weight-usually 1-3 pounds over several months. That’s one reason they’re still used in obese patients.
Can I take these drugs with metformin?
Yes, many people take acarbose or miglitol along with metformin. They work in different ways. Metformin reduces liver sugar production and improves insulin sensitivity. Alpha-glucosidase inhibitors slow carb digestion. Together, they can give better post-meal control. But combining them increases the risk of GI side effects, so your doctor will likely start you on a lower dose of the alpha-glucosidase inhibitor.
Why do these drugs only work if taken with meals?
They need to be in your small intestine at the exact moment your meal arrives. That’s when the enzymes are actively breaking down carbs. If you take them 15 minutes before eating, they’re not as effective. A 2021 study showed taking them with the first bite of food improved blood sugar control by 37% compared to taking them before the meal.
Are there any foods I should completely avoid?
Avoid simple sugars and refined carbs: white bread, pastries, sugary drinks, potatoes, and candy. These cause the most severe side effects. Also avoid high-fat meals-fat slows digestion, letting more carbs reach your colon. Stick to whole grains, legumes, vegetables, and lean proteins.
How long does it take for the side effects to get better?
Most people notice improvement after 6-8 weeks. By 12 weeks, about 70% report significantly less gas and bloating as their gut bacteria adapt. Don’t give up too soon-but if you’re still in severe discomfort after 3 months, talk to your doctor about switching.
Final Thoughts
Alpha-glucosidase inhibitors are a blunt tool. They work, but they come with a price. The side effects are real, common, and often underestimated by doctors who haven’t seen how hard they hit daily life. But they’re not hopeless. With the right diet, slow dosing, and patience, many people get through it. Others find better options. Either way, you don’t have to suffer in silence. Talk to your care team. Adjust your meals. Give it time-or switch. Your gut will thank you.

10 Comments
This is such a helpful breakdown! I was about to quit acarbose until I tried the slow-dose method - game changer. Your tips on whole grains and simethicone saved me.
It is worth noting, with a degree of scientific rigor, that the pharmacokinetic profile of alpha-glucosidase inhibitors renders them uniquely unsuitable for populations with high glycemic index dietary patterns, unless meticulously managed. The microbiome adaptation window, while statistically significant, remains clinically intolerable for a nontrivial subset of patients. One must question whether the marginal HbA1c benefit justifies the quality-of-life erosion - particularly when SGLT2 inhibitors offer superior outcomes with fewer gastrointestinal trade-offs.
Just wanted to say - you’re not alone. I was on this for 3 months and thought I was losing my mind. Then I switched to lentils and quinoa, started taking Gas-X before dinner, and now I can actually go out on weekends. It’s not perfect, but it’s doable. You got this 💪
I cried in the grocery store last week because I couldn’t eat a bowl of rice without feeling like I was going to explode. My husband said, ‘Maybe it’s not the rice, maybe it’s the drug.’ I didn’t want to hear it. But he was right. I’m switching. No more suffering for a 10-point drop in post-meal sugar.
One must interrogate the epistemological framework underpinning the medical establishment’s continued endorsement of these agents. The data is clear: they are obsolete. Their persistence is not a function of efficacy, but of institutional inertia, pharmaceutical lobbying, and the pathological aversion to prescribing newer, costlier alternatives. The patient’s gut is not a sacrificial altar to pharmacological tradition.
Y’all need to try the probiotic combo I’m on - L. acidophilus + B. lactis, 10 billion CFU, taken with breakfast. My gas went from ‘fire alarm in a subway’ to ‘quiet burp at dinner.’ Also, DO NOT SKIP MEALS. I did it once. My colon staged a coup. 🤯 Seriously, take this drug WITH food. It’s not a suggestion, it’s a commandment. And yes, I’m still on it. 6 months in. No more nightmares about public restrooms. 🙌
In India we use this drug because metformin causes liver issues and GLP1 is too expensive. Rice is our staple so acarbose works. No need to overcomplicate. Start low. Eat dal and roti. Avoid sugar. Done.
OMG I JUST REALIZED I WAS TAKING IT BEFORE MY MEAL 😭 I THOUGHT IT WAS LIKE METFORMIN. NO WONDER I WAS A HUMAN BALLOON. JUST STARTED TAKING IT WITH BITE OF FOOD AND MY GUT IS LIKE ‘THANK U 4 LISTENING’ 🙏🏻 also swapped white rice for brown and now i can sit through family dinners without hiding in the bathroom. love u post
So let me get this straight - you’re telling me I have to give up my favorite comfort foods… and eat ‘lentils’… just so I can avoid a 20-point sugar spike? And this is considered ‘medicine’? I miss the days when doctors just said ‘eat less cake’.
My husband took this for 2 weeks and said it felt like his intestines were hosting a rave. I told him to quit. He said ‘but the doctor said it’s good for my heart!’ I said ‘honey, your heart is fine - your colon is in crisis.’ We switched to empagliflozin. Now he’s losing weight, no gas, and we’re actually having sex again. 🙏