
Dosing Adjustment Calculator for Acarbose and Miglitol
Start Low, Go Slow Calculator
Based on clinical guidelines, this tool helps determine when to safely increase your dose to minimize GI side effects while maintaining blood sugar control.
Your Next Step
When to Increase Dose: -
Symptom Improvement Timeline: -
Based on clinical studies, most people see significant improvement by week 8.
How This Works
Start Low: Begin with 25 mg three times daily with your first bite of each meal. Stay at this dose for 2-4 weeks.
Go Slow: Only increase to the next dose level after 2-4 weeks if you're tolerating the current dose with mild or no symptoms.
Why it matters: This slow titration cuts discontinuation rates from 30% down to about 12% and allows your gut microbiome to adapt.
When you're managing type 2 diabetes, the last thing you want is to spend your day avoiding social situations because of constant bloating, cramps, or embarrassing gas. Yet for many people taking acarbose or miglitol, that’s exactly what happens. These drugs help control blood sugar after meals, but they come with a trade-off: gastrointestinal side effects that can be tough to live with. The good news? You don’t have to suffer through them forever. With the right approach, most people see major improvement in just a few weeks.
Why These Drugs Cause Gas and Bloating
Acarbose and miglitol belong to a class of drugs called alpha-glucosidase inhibitors. They work by slowing down how fast your body breaks down carbohydrates in the small intestine. That means more carbs reach your colon undigested. Bacteria in your colon feast on those carbs-and when they do, they produce gas. Lots of it. This isn’t a flaw in the drug. It’s how they’re supposed to work. The goal is to keep your blood sugar from spiking after meals. But because the undigested carbs don’t get absorbed up top, they end up fermenting down below. That’s where the bloating, cramps, and flatulence come from. Here’s the key difference between the two: acarbose stays mostly in your gut and doesn’t get absorbed into your bloodstream. That means it’s working hard right where the digestion happens-your upper intestine. Miglitol, on the other hand, gets absorbed about half the time. That means less of it stays behind to interact with gut bacteria, which is why miglitol tends to cause fewer side effects. Studies show that about 60-70% of people on acarbose report gas and bloating in the first few weeks. With miglitol, that number drops to around 50%. And while both drugs lower HbA1c by about 0.5% to 1%, acarbose has a slight edge in long-term glucose control-but only if you can stick with it.The First 30 Days: What to Expect
Most people hit their worst symptoms between days 3 and 7. That’s when your gut bacteria are suddenly flooded with undigested carbs they weren’t prepared for. You might feel like you’re constantly bloated, need to burp or pass gas constantly, or even get mild cramps. But here’s what most people don’t tell you: it gets better. By week 2 to 4, your gut microbiome adapts. The bacteria shift their population to handle the extra carbs. Gas production drops. Bloating eases. Many users on Reddit and diabetes forums say they barely notice symptoms after two months-if they stuck with it. A 2016 meta-analysis of over 3,000 patients found that nearly 30% quit these drugs within 12 weeks because the side effects felt unbearable. But those who stuck with it? Over 80% reported significant improvement by week 8. The key? Patience and smart adjustments.Dosing: Start Low, Go Slow
One of the biggest mistakes people make is starting at the full dose. That’s like throwing a whole bag of beans into your gut all at once. Instead, begin low. For both acarbose and miglitol, start with 25 mg three times a day-with the first bite of each meal. That’s the lowest available dose. Stay there for 2 to 4 weeks. Then, if you’re tolerating it, bump up to 50 mg. Wait another 2 to 4 weeks before going to 100 mg. Most people find they don’t need the full dose to get good blood sugar control. This slow titration cuts discontinuation rates in half-from 30% down to about 12%. It gives your gut time to adjust. And it’s not just theory: clinical guidelines from the American Diabetes Association and the American Association of Clinical Endocrinologists specifically recommend this approach.
Diet Tweaks That Make a Big Difference
What you eat matters just as much as how you take the drug. The more carbs you eat at once, the more gas you’ll produce. Avoid large meals packed with white bread, pasta, rice, potatoes, or sugary snacks. Instead, aim for consistent, moderate carb intake: 45 to 60 grams per meal. Spread your carbs evenly across breakfast, lunch, and dinner. That way, your gut isn’t overwhelmed at any one time. Also, cut back on high-fiber foods during the first few weeks. Beans, lentils, broccoli, and whole grains are healthy-but they’re also fermentable. Save them for later, once your gut has adapted. You can always add them back in slowly. And here’s something surprising: avoid sugary drinks and candy. Acarbose and miglitol don’t block sugar absorption like they do complex carbs. So if you drink soda or eat candy, your blood sugar will still spike-and you’ll still get gas. These drugs only slow down starch digestion, not simple sugars.Over-the-Counter Helpers
If you’re still struggling, there are a few OTC options that actually work:- Simethicone (Gas-X, Mylanta Gas): Helps break up gas bubbles. Take 120 mg three times a day with meals. One study showed it reduced bloating by 40%.
- Activated charcoal: Can bind to gas-producing compounds. Take 500 mg 30 minutes before meals. Studies found it cuts flatus volume by about a third.
- Probiotics: Specifically, Lactobacillus GG or Bifidobacterium longum BB536. A 2023 study showed BB536 reduced flatulence by 42% when taken with miglitol. Look for supplements with at least 10 billion CFUs daily.
Acarbose vs. Miglitol: Which Is Easier on Your Gut?
If you’re choosing between the two, miglitol usually wins for tolerability. In a direct head-to-head study of 20 men, miglitol caused significantly less gas and bloating than acarbose-even when both were at the same dose. Why? Because miglitol gets absorbed into the bloodstream more. That means less of it lingers in the gut to feed bacteria. Acarbose stays put-so it’s more effective at slowing carbs, but also more likely to cause side effects. If you’ve tried acarbose and it felt unbearable, switching to miglitol might be your best move. Many endocrinologists now recommend miglitol as the preferred AGI for patients with sensitive stomachs.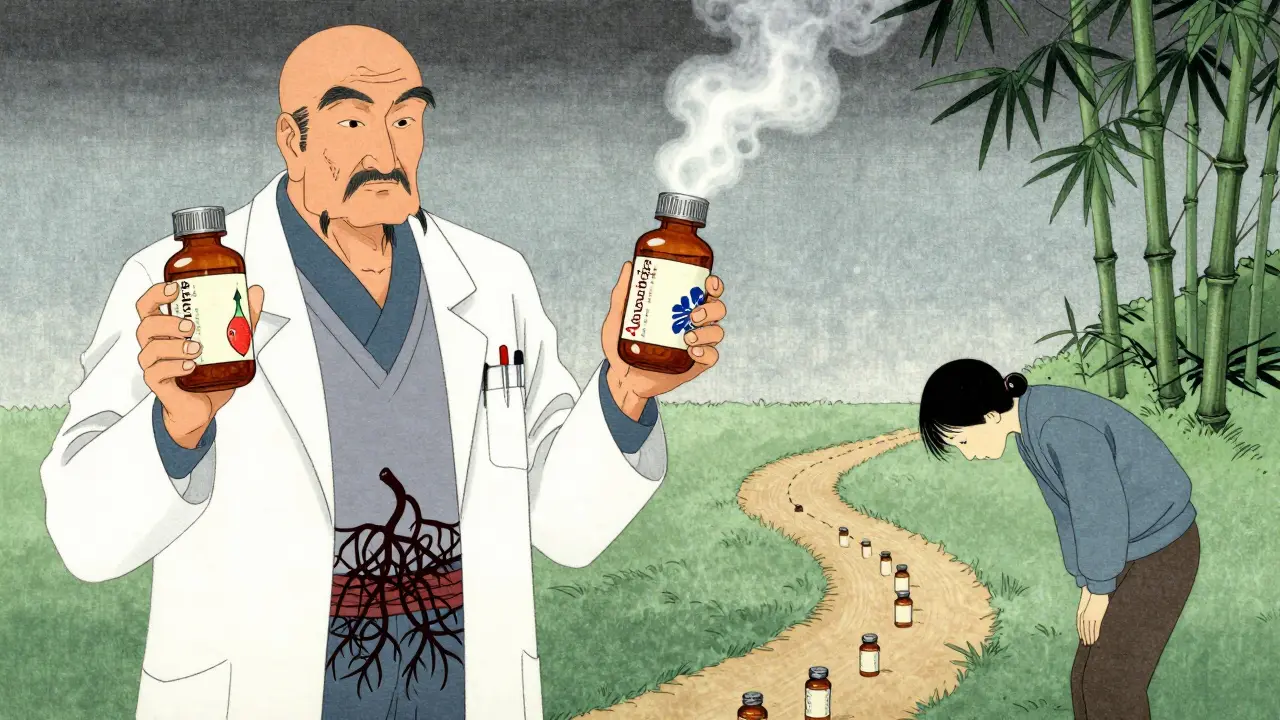
When to Talk to Your Doctor
Most GI side effects are annoying, not dangerous. But call your doctor if you experience:- Severe abdominal pain
- Swelling in your face, lips, or throat
- Yellowing of skin or eyes (signs of liver issues-rare with acarbose)
- Diarrhea that lasts more than a week
Is It Worth It?
Let’s be honest: these drugs aren’t glamorous. They don’t come with flashy marketing or celebrity endorsements. But they do something few other diabetes meds can: lower blood sugar without making you gain weight or risking low blood sugar. For someone who’s overweight and can’t take metformin, or who wants to avoid insulin, acarbose and miglitol can be lifesavers. In Japan, where diets are high in rice and carbs, these drugs are first-line treatments. And they work. The real question isn’t whether they’re effective. It’s whether you can stick with them long enough for your gut to catch up. For most people, the answer is yes.What’s Next for These Drugs?
New developments are making these drugs easier to use. In 2023, the FDA approved a new combination pill-Acbeta-M-that blends acarbose with metformin in a controlled-release formula. Early results show 28% less gas than regular acarbose. Researchers are also exploring genetic tests that could predict who’s more likely to have bad side effects. If your gut enzymes are naturally slower, you might respond better to these drugs-or worse. Personalized dosing could be the future. For now, the best advice is simple: start low, go slow, tweak your diet, use OTC help if needed, and give it time. Your gut will thank you.How long does gas from acarbose or miglitol last?
Most people experience peak gas and bloating between days 3 and 7 after starting the medication. Symptoms usually improve noticeably by week 2 to 4, and many users report minimal issues after 8 to 12 weeks as gut bacteria adapt to the undigested carbs.
Can I take simethicone or activated charcoal with these drugs?
Yes. Simethicone (120 mg three times daily) and activated charcoal (500 mg 30 minutes before meals) are safe to use alongside acarbose and miglitol. Both have been shown in clinical studies to reduce bloating and flatus without interfering with blood sugar control.
Why is miglitol better than acarbose for gas?
Miglitol is absorbed about 50-100% in the upper intestine, so less of it remains to feed gut bacteria. Acarbose is barely absorbed and stays in the gut longer, increasing fermentation and gas production. Studies show miglitol causes significantly less flatulence and bloating at equivalent doses.
Should I avoid fiber while taking these drugs?
During the first 2 to 4 weeks, reduce high-fiber foods like beans, lentils, broccoli, and whole grains. These foods ferment easily and can worsen gas. Once your gut adapts, you can slowly reintroduce them. Consistent, moderate fiber is still important for long-term health.
Do these drugs cause weight gain?
No. Unlike insulin or sulfonylureas, acarbose and miglitol are weight-neutral. In fact, miglitol has been shown in studies to cause a small weight loss-about 1.2 kg over 12 weeks-because undigested carbs pass through without being absorbed as calories.
What if I can’t tolerate either drug?
Many people switch to metformin, SGLT2 inhibitors (like dapagliflozin), or GLP-1 agonists (like semaglutide). These alternatives don’t cause gas and often offer additional benefits like weight loss or heart protection. Talk to your doctor about what fits your goals.
Can I take these drugs with other diabetes medications?
Yes. Acarbose and miglitol are often combined with metformin, DPP-4 inhibitors, or even insulin. In fact, the new Acbeta-M pill combines acarbose and metformin in one tablet to improve tolerability. Always check with your doctor before combining medications.
Is it safe to take these drugs long-term?
Yes. Both drugs have been used safely for over 25 years. Long-term studies show no increased risk of liver damage, kidney problems, or cancer. The FDA issued a rare warning about liver enzyme elevations with acarbose (0.02% incidence), but this is extremely uncommon and reversible if caught early.

1 Comments
I started acarbose last month and honestly thought I was going to lose my mind. Day 4 was brutal-like, constant noise and bloating that made me cancel plans. But I stuck with the 25mg dose for three weeks before bumping up. By week 5, it was night and day. I still get a little gassy after pasta, but now I just laugh it off. Pro tip: skip the rice bowls. Swap them for quinoa and roasted veggies. Game changer.
Also, the Lactobacillus GG probiotic I got from the health store? Total lifesaver. Not magic, but it took the edge off.